Introduction
Cerebral malaria is one of the deadliest forms of Plasmodium falciparum infection, affecting both children and adults. It’s a medical emergency characterized by fever, coma, and neurological symptoms due to malaria parasites invading the brain.
In India, where malaria remains endemic in several states, understanding the clinical drivers of outcomes in cerebral malaria helps doctors improve diagnosis, treatment, and survival rates.
This blog explores what cerebral malaria is, how it affects the brain, key outcome predictors, available treatments, and how early care can save lives.

Overview of Cerebral Malaria
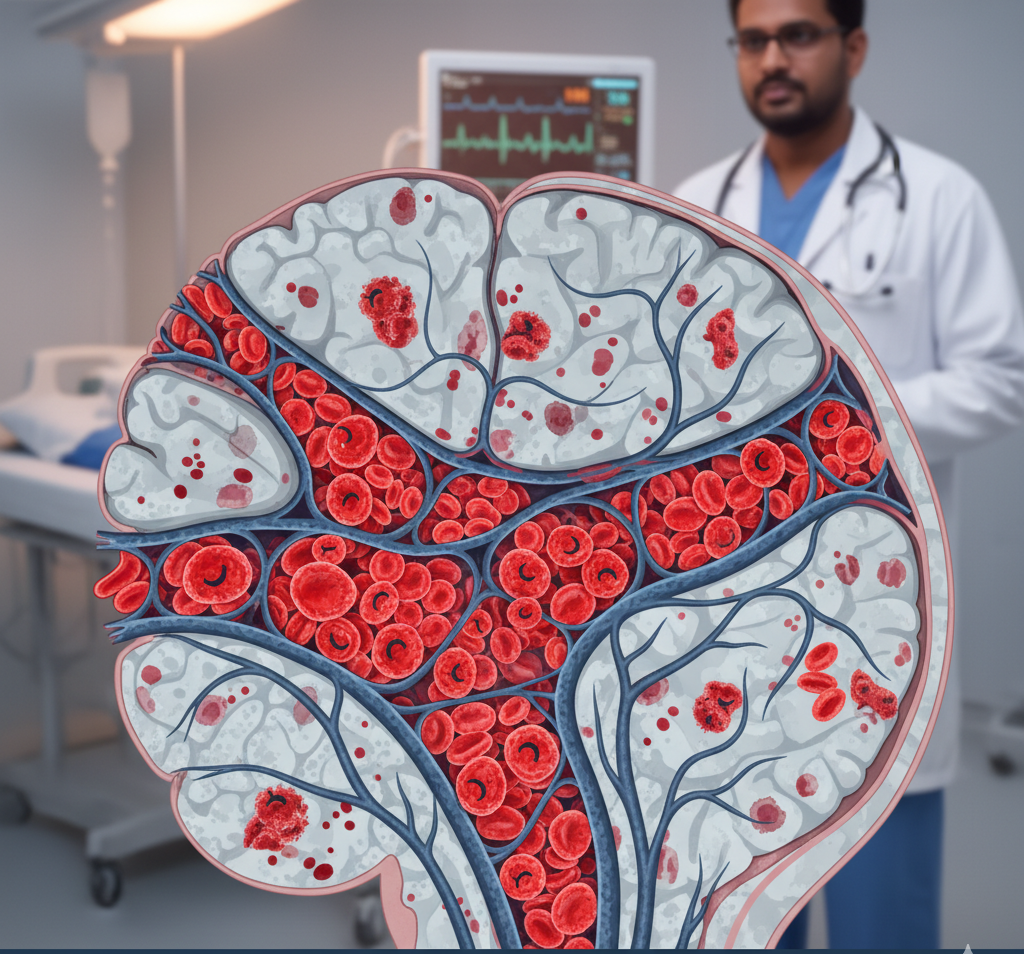
Cerebral malaria is a severe manifestation of Plasmodium falciparum malaria that causes inflammation and blockage of tiny blood vessels in the brain. The result is brain swelling, seizures, confusion, and loss of consciousness.
It is most common among children under five and adults in malaria-endemic regions like Northeast India, Odisha, Jharkhand, and Chhattisgarh.
Key features:
-
High fever with chills
-
Coma or unresponsiveness
-
Recurrent seizures
-
Abnormal posturing
-
Respiratory distress or shock
Untreated cerebral malaria has a mortality rate of up to 20–30%, even with intensive care.
Causes and Pathophysiology
1. Role of Plasmodium falciparum
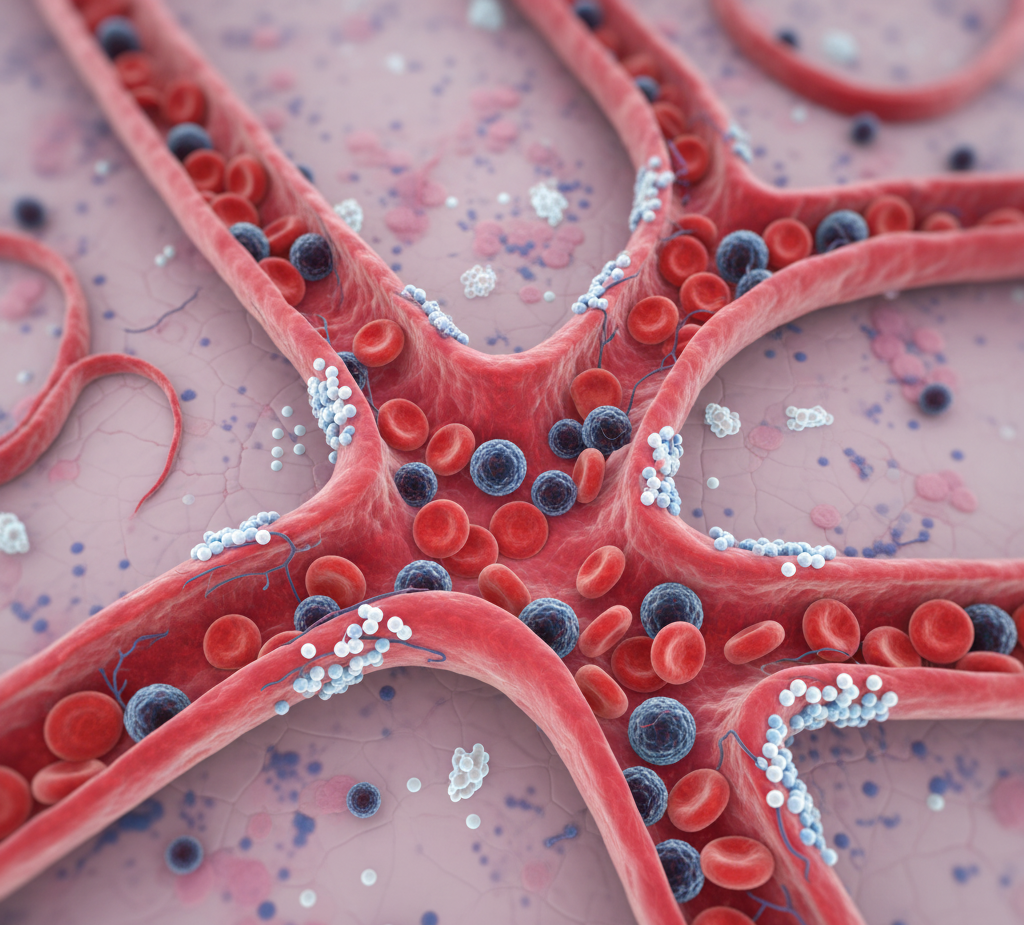
Among malaria parasites, Plasmodium falciparum is most virulent. It infects red blood cells (RBCs), making them sticky and causing them to clump inside small brain capillaries—a process called sequestration.
2. Brain Inflammation
When infected RBCs block brain vessels, oxygen supply drops and inflammation increases. Cytokines like TNF-alpha and IL-1β damage brain tissue, leading to edema and dysfunction of the blood–brain barrier.
3. Microvascular Obstruction
Severe blockage in cerebral vessels leads to:
-
Reduced oxygen delivery
-
Lactic acidosis
-
Brain swelling and raised intracranial pressure
4. Systemic Factors
Anemia, hypoglycemia, acidosis, and multi-organ failure further worsen prognosis.
Clinical Drivers of Outcome
1. Parasite Load (Parasitemia)
Higher levels of P. falciparum in blood are directly linked with poor survival. A parasite density >5% of RBCs infected is associated with severe disease.
2. Duration of Coma
The longer a patient remains unconscious, the poorer the neurological outcome. Early intervention (within 24 hours of symptoms) improves chances of recovery.
3. Seizures and Neurological Complications
Frequent or prolonged seizures increase brain damage risk and may lead to residual neurological deficits, especially in children.
4. Systemic Organ Failure
-
Renal failure: Common in adults with severe malaria.
-
Liver dysfunction: Causes jaundice and coagulopathy.
-
Respiratory distress: Indicates poor prognosis.
5. Blood–Brain Barrier Damage
Leakage of plasma and immune cells into brain tissue increases cerebral edema, worsening coma depth and duration.
6. Hypoglycemia and Metabolic Acidosis
These are common in severe malaria and can mimic worsening coma, often contributing to death if unrecognized.
7. Anemia and Hypoxia
Low hemoglobin reduces oxygen delivery to the brain, compounding cerebral injury.
8. Delay in Treatment
Each hour of delay after onset of coma increases mortality risk. Early diagnosis and parenteral antimalarial therapy are crucial.

Diagnosis
1. Clinical Evaluation
-
Unconsciousness not explained by other causes
-
History of fever or malaria exposure
-
Seizures, abnormal posture, or breathing patterns
2. Laboratory Tests
-
Peripheral smear or rapid antigen test: Detects P. falciparum.
-
Blood glucose: To rule out hypoglycemia.
-
Electrolytes and renal function: To monitor organ involvement.
-
Lumbar puncture: To rule out meningitis.
3. Imaging (CT/MRI)
Used in specialized centers to detect brain edema, hemorrhage, or ischemia.
Treatment
1. Emergency Antimalarial Therapy
-
Intravenous artesunate is the first-line treatment for all severe and cerebral malaria cases.
-
If unavailable, quinine or artemether may be used.
-
Duration: 7–10 days or until full recovery.
2. Supportive Care
-
Maintain airway and breathing.
-
Correct hypoglycemia with dextrose.
-
Control seizures using diazepam or phenobarbital.
-
Manage fluids carefully to avoid brain swelling.
-
Treat anemia with blood transfusion if severe.
3. Management of Organ Failure
-
Dialysis for renal failure.
-
Oxygen therapy or ventilation for respiratory distress.
-
Liver support in cases with jaundice or coagulation abnormalities.
4. Monitoring and Follow-up
Neurological recovery may take weeks. Some patients develop long-term complications like cognitive deficits or motor weakness.
Lifestyle and Recovery Support
-
Rest and nutritious diet during recovery.
-
Iron- and folate-rich foods for anemia correction.
-
Physiotherapy for movement problems.
-
Regular check-ups with a neurologist or general physician.
Prevention Strategies
-
Use insecticide-treated bed nets (ITNs).
-
Indoor residual spraying in malaria-prone areas.
-
Early diagnosis and prompt treatment of all malaria cases.
-
Prophylactic medication for travelers to endemic regions.
-
Public health education on mosquito control and hygiene.
When to See a Doctor
Seek medical help immediately if you or someone you know experiences:
-
High fever with confusion or unconsciousness
-
Seizures or abnormal movements
-
Jaundice, breathing difficulty, or reduced urine
-
Weakness or unresponsiveness after fever
Risks and Complications
Untreated or severe cerebral malaria can lead to:
-
Brain swelling and coma
-
Seizures and memory issues
-
Organ failure
-
Death in 20–30% of cases
Children may have long-term effects like speech or learning difficulties.
Conclusion
Cerebral malaria remains a medical emergency that demands quick hospital care. Early diagnosis, intravenous antimalarial therapy, and supportive treatment reduce death rates significantly.
Clinical drivers such as parasite load, coma duration, and organ failure are critical indicators guiding prognosis.
Raising awareness and improving access to healthcare in endemic regions can help save countless lives.
Quickobook CTA
If you or a loved one shows signs of severe malaria or neurological symptoms, don’t delay — book an appointment with a doctor on Quickobook today.
Quickobook connects you to verified physicians and specialists across India for fast consultations, lab testing, and emergency guidance.
Frequently Asked Questions (50 FAQs)
Q1. What is cerebral malaria?
A. Cerebral malaria is a severe form of Plasmodium falciparum infection affecting the brain, leading to coma and neurological symptoms.
Q2. Which parasite causes cerebral malaria?
A. Plasmodium falciparum is responsible for cerebral malaria.
Q3. How does cerebral malaria affect the brain?
A. It causes blockage of small brain vessels and inflammation, leading to swelling and impaired function.
Q4. Who is at highest risk of cerebral malaria?
A. Children under five, pregnant women, and adults in endemic areas are at high risk.
Q5. Is cerebral malaria contagious?
A. No, it spreads through mosquito bites, not from person to person.
Q6. What are early symptoms of cerebral malaria?
A. High fever, headache, vomiting, and confusion are common early signs.
Q7. Can cerebral malaria cause seizures?
A. Yes, seizures are a frequent and serious complication.
Q8. How quickly can cerebral malaria develop?
A. It can progress within hours or days after infection.
Q9. Is cerebral malaria curable?
A. Yes, with early diagnosis and proper treatment, it can be cured.
Q10. What drug is used for treatment?
A. Intravenous artesunate is the first-line treatment.
Q11. How long does treatment take?
A. Usually 7–10 days, depending on severity.
Q12. What happens if treatment is delayed?
A. Delay increases risk of death or permanent brain damage.
Q13. Can cerebral malaria cause coma?
A. Yes, prolonged unconsciousness is a hallmark feature.
Q14. How is cerebral malaria diagnosed?
A. By blood tests detecting P. falciparum and clinical evaluation.
Q15. Is CT or MRI needed?
A. Sometimes used to detect brain swelling or bleeding.
Q16. What is the mortality rate?
A. About 20–30% in severe cases, even with treatment.
Q17. What are neurological sequelae?
A. Long-term effects like weakness, memory loss, or epilepsy.
Q18. Can cerebral malaria recur?
A. Rarely, but reinfection can occur if exposed again.
Q19. Is there a vaccine?
A. The RTS,S vaccine helps prevent malaria but not specifically cerebral malaria.
Q20. Can anemia worsen cerebral malaria?
A. Yes, low hemoglobin reduces oxygen delivery to the brain.
Q21. What is parasite load?
A. It’s the number of malaria parasites in the blood, influencing disease severity.
Q22. Why does brain swelling occur?
A. Due to inflammation and blocked blood flow in the brain.
Q23. Can cerebral malaria cause blindness?
A. In rare cases, optic nerve damage may occur.
Q24. What organs are affected?
A. Brain, kidneys, liver, and lungs are commonly affected.
Q25. Is cerebral malaria more common in India?
A. Yes, in states like Odisha, Jharkhand, Chhattisgarh, and Assam.
Q26. Can it affect pregnant women?
A. Yes, it can cause severe complications for both mother and baby.
Q27. How is hypoglycemia related?
A. Low blood sugar is common in severe malaria and worsens prognosis.
Q28. What are warning signs of poor outcome?
A. Deep coma, multiple seizures, organ failure, and high parasite count.
Q29. What should caregivers watch for?
A. Unresponsiveness, rapid breathing, or persistent fever.
Q30. Can children recover completely?
A. Many recover fully with early care, though some may have learning issues.
Q31. Can cerebral malaria cause stroke?
A. Rarely, due to blood vessel blockage in the brain.
Q32. What lab tests confirm malaria?
A. Peripheral smear or rapid diagnostic tests.
Q33. Can it be mistaken for meningitis?
A. Yes, symptoms can overlap; lab tests help differentiate.
Q34. How can you prevent malaria?
A. By avoiding mosquito bites using nets, repellents, and spraying.
Q35. What is the role of the immune system?
A. Strong immunity helps control infection and reduce severity.
Q36. Can cerebral malaria cause memory loss?
A. Yes, temporary or long-term memory problems can occur.
Q37. Are steroids used in treatment?
A. No, corticosteroids are not recommended as they worsen outcomes.
Q38. What type of doctor treats cerebral malaria?
A. Infectious disease specialists, neurologists, and ICU doctors.
Q39. Can rural hospitals manage it?
A. Severe cases should be referred to tertiary hospitals with ICU support.
Q40. Can blood transfusion help?
A. Yes, in cases with severe anemia.
Q41. How to detect organ failure early?
A. Regular monitoring of kidney and liver function tests.
Q42. Can cerebral malaria be fatal?
A. Yes, without treatment it can lead to death.
Q43. Is it more severe in children?
A. Yes, children develop symptoms faster and may deteriorate quickly.
Q44. Does nutrition affect recovery?
A. Yes, adequate nutrition supports healing and immune strength.
Q45. Can oxygen therapy help?
A. Yes, it improves brain oxygenation in severe cases.
Q46. What is post-malaria syndrome?
A. A condition with weakness, fatigue, or mood changes after recovery.
Q47. Is rehabilitation needed after coma?
A. Sometimes, physiotherapy or counseling may be required.
Q48. How long does full recovery take?
A. It varies — from weeks to months depending on severity.
Q49. Can cerebral malaria cause hearing loss?
A. Rarely, if brainstem regions are affected.
Q50. When should I seek emergency care?
A. If someone with fever becomes drowsy, confused, or has seizures — seek help immediately.






Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment