Introduction
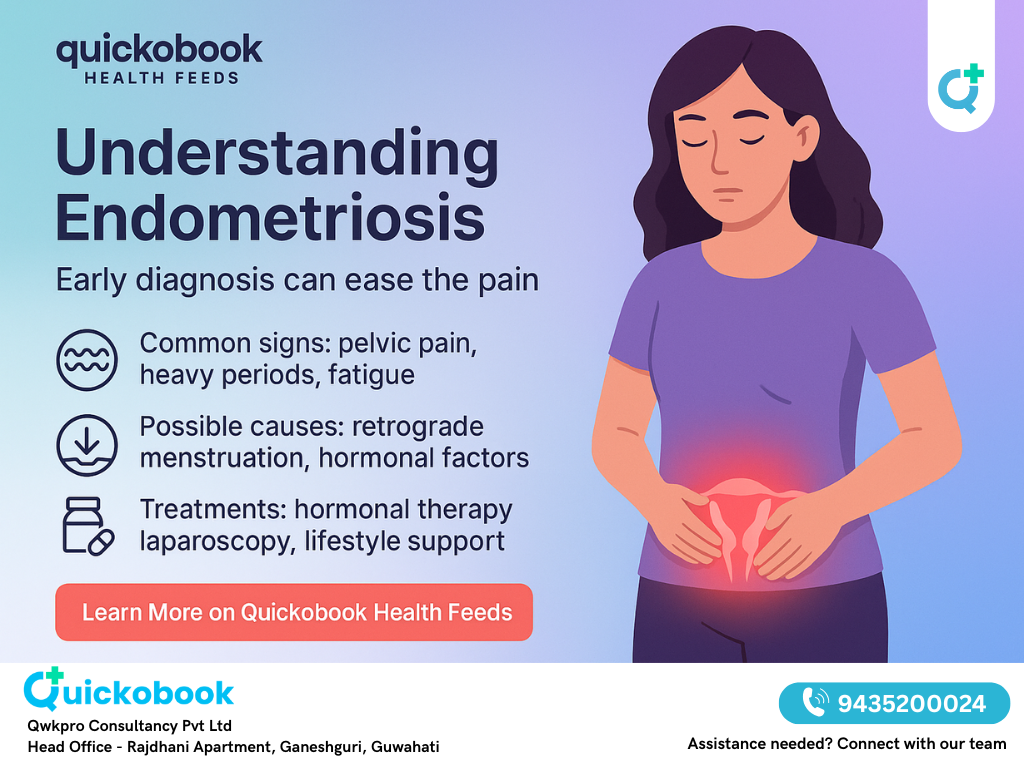
Endometriosis is a common yet underdiagnosed condition affecting millions of women in India. It occurs when tissue similar to the lining of the uterus grows outside it, leading to severe period pain, pelvic discomfort, and even infertility. Many women delay seeking medical help due to stigma or considering pain as "normal." Consulting a Gynaecologist early can make a huge difference in management and quality of life.
What is Endometriosis?
Endometriosis is a chronic gynaecological disorder where endometrial-like tissue grows outside the uterus. These tissues respond to monthly hormonal changes, causing inflammation, bleeding, and scarring.
Key facts:
- Affects women in their reproductive years (15–49 years).
- Can impact ovaries, fallopian tubes, pelvic lining, and bowel.
- Often linked with infertility and chronic pain.
Causes of Endometriosis
The exact cause is still unknown, but possible explanations include:
- Retrograde menstruation – menstrual blood flows backward into the pelvis.
- Genetics – family history increases risk.
- Immune dysfunction – the body fails to destroy misplaced tissue.
- Hormonal imbalance – excess estrogen can fuel endometriosis growth.
Signs and Symptoms
Many women mistake symptoms for normal menstrual discomfort. Common signs include:
- Severe period pain (dysmenorrhea).
- Pain during intercourse.
- Chronic pelvic pain.
- Heavy or irregular periods.
- Fatigue and low energy.
- Difficulty in conceiving.
- Painful urination or bowel movements during menstruation.
Diagnosis
A Gynaecologist may suggest the following to confirm endometriosis:
- Medical history & pelvic exam
- Ultrasound / MRI for cysts
- Laparoscopy (minimally invasive surgery) – gold standard for diagnosis
Treatment Approaches
Treatment depends on severity, age, and fertility goals.
1. Medications
- Pain relievers (NSAIDs like ibuprofen)
- Hormonal therapy – birth control pills, IUDs, or injections to control estrogen
- GnRH agonists – to suppress endometriosis tissue growth
2. Surgery
- Laparoscopy – to remove or destroy lesions
- Hysterectomy – in severe cases where other treatments fail
3. Fertility Management
- IVF (In Vitro Fertilization) can help women struggling with infertility due to endometriosis.
Lifestyle and Home Care
- Exercise regularly – improves blood flow and reduces pain.
- Balanced diet – anti-inflammatory foods like fruits, vegetables, and omega-3.
- Heat therapy – warm compress or hot water bag for pain relief.
- Stress management – yoga, meditation, and adequate sleep.
Prevention and Risk Reduction
Endometriosis cannot always be prevented, but early detection helps. Regular check-ups with a gynaecologist and tracking period pain patterns are crucial.
When to See a Gynaecologist
Consult a gynaecologist if you experience:
- Severe period pain that affects daily life.
- Pain during sex or bowel movements.
- Heavy bleeding or irregular cycles.
- Infertility despite trying for over a year.
READ ALSO: Premenstrual Syndrome (pms) – Signs, Symptoms, And Relief Strategies
Risks and Complications
- Infertility
- Ovarian cysts (endometriomas)
- Adhesions and scar tissue
- Chronic pelvic pain
- Higher risk of ovarian cancer in rare cases
Conclusion
Endometriosis is not "just bad period pain." It is a chronic condition that needs timely diagnosis and treatment. Women must not ignore their symptoms and should seek guidance from a gynecologist. With medical support, lifestyle changes, and awareness, living a healthy and fulfilling life with endometriosis is possible.
FAQs – Endometriosis in Women (50 Expert Answers)
Q1. Is severe period pain always a sign of endometriosis?
A. Not always, but intense pain interfering with daily activities should be checked by a gynaecologist.
Q2. Can endometriosis cause pain outside periods?
A. Yes, women may experience pelvic pain during ovulation, urination, or sex, not just menstruation.
Q3. Is fatigue a symptom of endometriosis?
A. Yes, many women report extreme tiredness due to chronic inflammation and pain.
Q4. Can endometriosis affect digestion?
A. Some women experience bloating, constipation, or diarrhea during periods due to pelvic involvement.
Q5. Is infertility a common symptom of endometriosis?
A. Around 30–40% of women with endometriosis may struggle with conception.
Q6. Does heavy bleeding indicate endometriosis?
A. Yes, many women have heavy or irregular menstrual bleeding as a symptom.
Q7. Can symptoms worsen over time?
A. Yes, untreated endometriosis can progress, leading to more severe pain and complications.
Q8. What age group is most affected by endometriosis?
A. Women in their reproductive years (15–49 years) are most commonly affected.
Q9. Can teenagers have endometriosis?
A. Yes, even adolescent girls can develop endometriosis, though diagnosis may be delayed.
Q10. Can endometriosis go away after menopause?
A. Symptoms often improve after menopause due to lower estrogen levels, but not always.
Q11. Can pregnancy cure endometriosis?
A. Pregnancy may reduce symptoms temporarily but does not cure endometriosis.
Q12. Is endometriosis hereditary?
A. Yes, having a family history increases your risk of developing the condition.
Q13. Can endometriosis return after surgery?
A. Yes, recurrence is possible, especially if only lesions are removed.
Q14. Does endometriosis increase cancer risk?
A. Rarely, but it can slightly increase the risk of ovarian cancer.
Q15. Can endometriosis cause weight gain?
A. Indirectly, due to hormonal therapy or reduced activity from chronic pain.
Q16. Can stress worsen endometriosis symptoms?
A. Yes, stress can trigger inflammation and pain flares.
Q17. Can exercise help manage endometriosis?
A. Yes, regular exercise reduces inflammation and relieves stress.
Q18. Are there foods that worsen endometriosis?
A. Processed foods, red meat, and excess caffeine may worsen symptoms.
Q19. Can yoga help with endometriosis pain?
A. Yes, yoga improves flexibility, reduces stress, and helps ease pelvic pain.
Q20. Does smoking affect endometriosis?
A. Yes, smoking increases inflammation and may worsen symptoms.
Q21. Can endometriosis cause back pain?
A. Yes, lower back pain is a common complaint in many women.
Q22. Does endometriosis always cause infertility?
A. No, many women with endometriosis conceive naturally, though fertility may be reduced.
Q23. Can an ultrasound always detect endometriosis?
A. No, smaller lesions may not be visible on ultrasound.
Q24. Is laparoscopy safe for diagnosing endometriosis?
A. Yes, it is a minimally invasive and reliable diagnostic procedure.
Q25. Can endometriosis be prevented?
A. No guaranteed prevention exists, but early treatment reduces complications.
Q26. Can birth control pills help with endometriosis?
A. Yes, they regulate hormones and reduce pain and bleeding.
Q27. Is an IUD helpful in endometriosis?
A. Yes, hormonal IUDs can reduce heavy bleeding and pain.
Q28. Can endometriosis cause anemia?
A. Yes, heavy bleeding can lead to iron-deficiency anemia.
Q29. Can men get endometriosis?
A. Rarely, men on high-dose estrogen therapy may develop it, but it’s extremely uncommon.
Q30. Can endometriosis spread to other organs?
A. Yes, though rare, it may affect the lungs or diaphragm.
Q31. Does endometriosis worsen with age?
A. It often worsens until menopause unless treated.
Q32. Can endometriosis affect mental health?
A. Yes, chronic pain may cause anxiety, depression, and stress.
Q33. Can endometriosis be cured completely?
A. Currently, there is no permanent cure, but treatments manage symptoms effectively.
Q34. Can acupuncture help endometriosis pain?
A. Some women report relief, but evidence is limited.
Q35. Can endometriosis be misdiagnosed as PCOS?
A. Yes, overlapping symptoms like irregular cycles can cause confusion.
Q36. Can endometriosis affect bladder health?
A. Yes, it can cause painful urination and frequent urgency during periods.
Q37. Is endometriosis a hormonal disease?
A. Yes, it is influenced by estrogen and other hormones.
Q38. Can fertility treatments bypass endometriosis-related infertility?
A. Yes, IVF and assisted reproductive techniques often help.
Q39. Can endometriosis cause early menopause?
A. Treatments like surgery or medication may induce temporary menopause-like states.
Q40. Does Ayurveda help endometriosis?
A. Some herbal remedies may relieve symptoms, but consult a doctor first.
Q41. Can endometriosis cause nausea?
A. Yes, nausea is a common symptom during painful periods.
Q42. Can sleep improve endometriosis symptoms?
A. Yes, good sleep reduces inflammation and pain sensitivity.
Q43. Does alcohol worsen endometriosis?
A. Yes, alcohol increases estrogen levels, which may worsen symptoms.
Q44. Can endometriosis be detected in blood tests?
A. No, there is no definitive blood test yet for diagnosis.
Q45. Can pregnancy tests be affected by endometriosis?
A. No, endometriosis does not affect pregnancy test results.
Q46. Can endometriosis cause hip pain?
A. Yes, pain may radiate to hips and thighs during menstruation.
Q47. Is weight loss beneficial for endometriosis?
A. Yes, maintaining healthy weight reduces inflammation and hormone imbalance.
Q48. Can endometriosis cause mood swings?
A. Yes, hormonal imbalance and chronic pain contribute to mood changes.
Q49. Can endometriosis affect sexual health?
A. Yes, pain during sex is a common symptom that affects intimacy.
Q50. Can a gynaecologist fully manage endometriosis?
A. Yes, a gynaecologist is the best specialist to diagnose, treat, and manage endometriosis.
Quickobook CTA
Looking for expert care? Book an appointment with a trusted gynaecologist near you on Quickobook. Get timely advice, treatment, and support for managing period pain and endometriosis effectively.
Disclaimer: This blog is for educational purposes only. It is not a substitute for professional medical advice. Always consult a gynaecologist for diagnosis and treatment of endometriosis.






Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment