Introduction
For decades, Type 1 diabetes has been viewed as a lifelong condition — one that requires constant insulin injections, strict monitoring, and disciplined dietary management. But a groundbreaking medical case has changed the landscape.
A man diagnosed with Type 1 diabetes has achieved something once thought impossible: his body began producing its own insulin again. This revolutionary result, made possible through advanced regenerative medicine, has opened the door to a potential functional cure for millions living with this chronic condition.
This Quickobook article explores the science behind this breakthrough, what it means for the future of Type 1 diabetes care, and how it may transform treatment approaches globally and in India.
Understanding Type 1 Diabetes
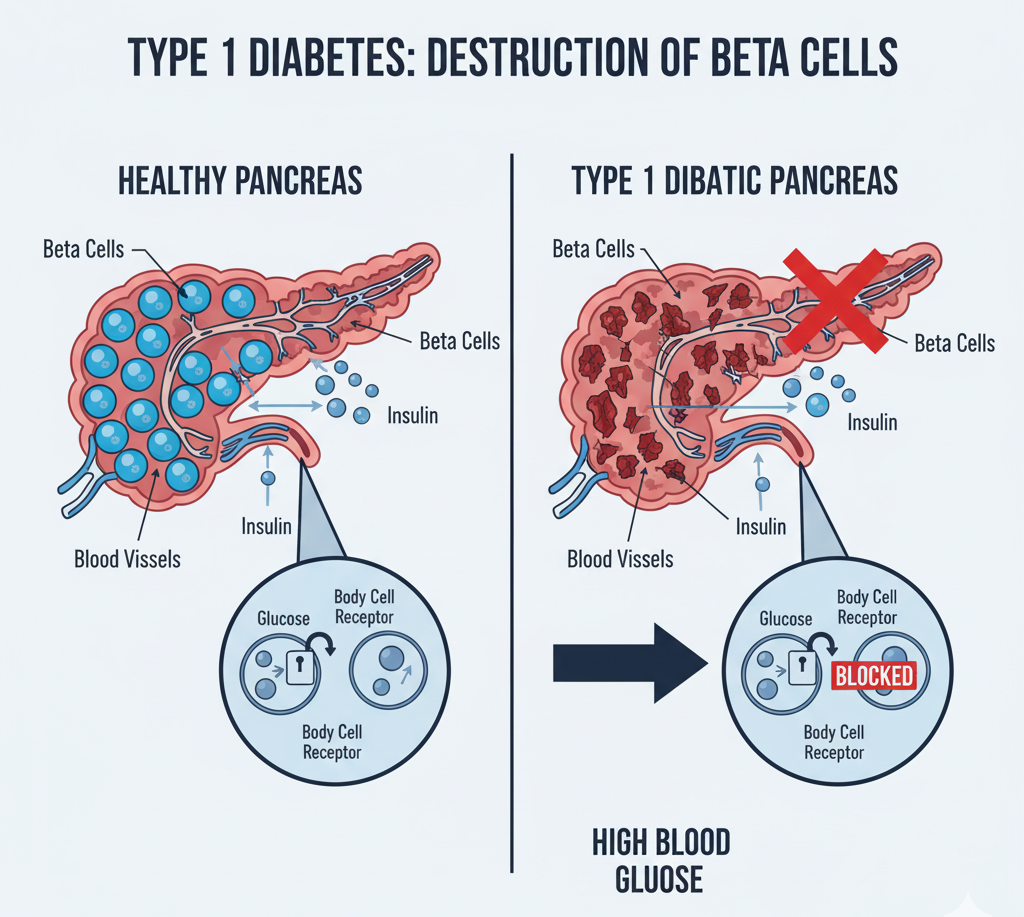
Type 1 diabetes (T1D) is an autoimmune disease in which the immune system mistakenly attacks the insulin-producing beta cells of the pancreas. Without insulin, glucose builds up in the blood, leading to serious complications affecting the heart, kidneys, eyes, and nerves.
Unlike Type 2 diabetes, which is often related to lifestyle factors such as obesity and inactivity, Type 1 diabetes usually develops in childhood or early adulthood and is not preventable.
Common Symptoms of Type 1 Diabetes
-
Excessive thirst and frequent urination
-
Sudden weight loss
-
Fatigue and blurred vision
-
Increased hunger
-
Slow-healing wounds
-
In severe cases: diabetic ketoacidosis (DKA)
For most patients, lifelong insulin therapy has been the only effective treatment — until now.
The Groundbreaking Case: Making Insulin Naturally Again
The medical breakthrough came from a clinical trial conducted in the United States, involving a stem cell-derived therapy designed to restore the pancreas’s natural ability to produce insulin.
One of the trial participants, a 64-year-old man diagnosed with Type 1 diabetes over 40 years ago, began producing measurable levels of insulin on his own for the first time since his diagnosis.
Doctors reported that:
-
His blood sugar levels stabilised without needing external insulin injections.
-
C-peptide levels, a marker of insulin production, rose significantly.
-
His HbA1c levels improved, indicating long-term glucose control.
This case represents the first real evidence that regenerative cell therapy can reverse insulin dependence in a person with Type 1 diabetes.
How Regenerative Medicine Made It Possible
The treatment used stem cell–derived pancreatic beta cells, developed using a patient’s own cells or donor stem cells. These were implanted into the patient’s body, where they began functioning like healthy pancreatic cells — producing and releasing insulin in response to blood sugar levels.
How It Works
-
Stem cell collection: Scientists harvest pluripotent stem cells capable of turning into any cell type.
-
Cell differentiation: These cells are programmed to become pancreatic islet cells (beta cells).
-
Implantation: The lab-grown cells are placed inside the patient’s body (often within a small bioengineered pouch).
-
Immune protection: A special encapsulation technology shields these cells from autoimmune attack.
-
Insulin regulation: Once integrated, the cells start producing insulin naturally.
This approach combines cell biology, immunology, and bioengineering — representing the true power of regenerative medicine.
Why This Discovery Is So Important
Type 1 diabetes affects an estimated 8.7 million people worldwide, including over 1.5 million in India. Despite technological advances in insulin pumps and glucose sensors, patients still face a daily burden of management.
The new regenerative therapy offers:
-
Freedom from daily insulin injections
-
Improved quality of life
-
Reduced long-term complications
-
Potential one-time treatment solution
If replicated in larger trials, this innovation could shift diabetes management from lifelong control to functional cure.
Other Advancements in Type 1 Diabetes Research
Several parallel developments are fueling optimism in the diabetes research community:
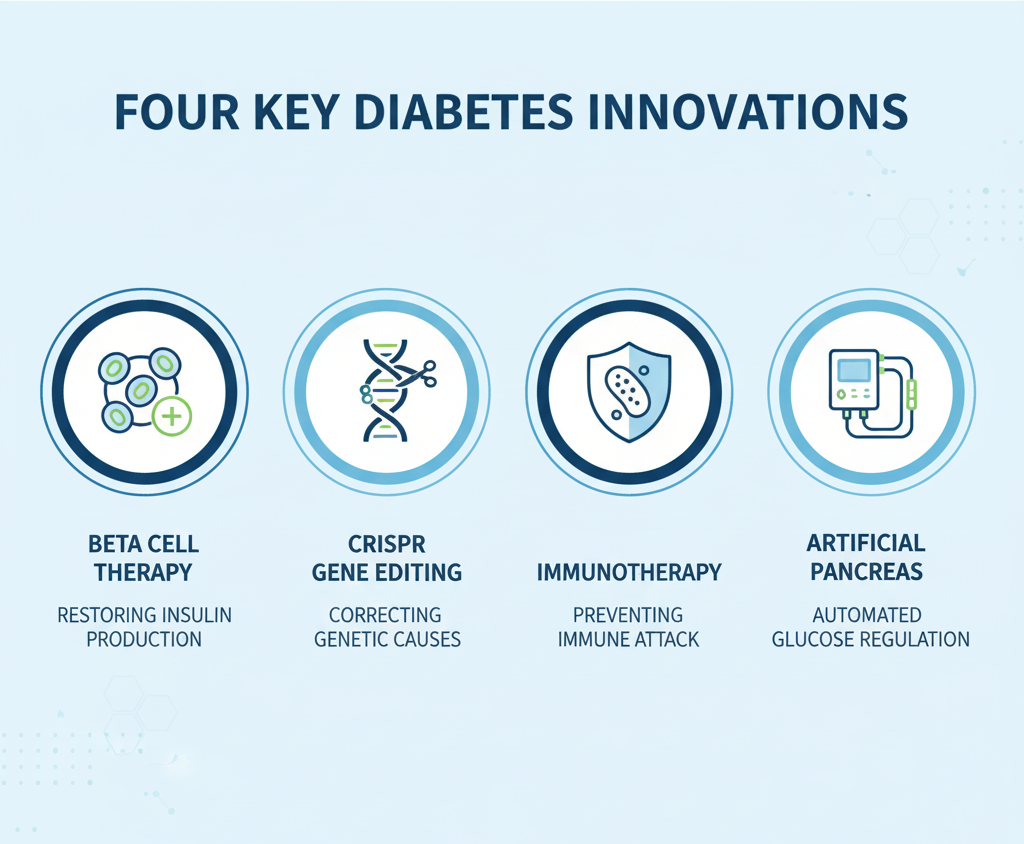
1. Beta Cell Replacement Therapy
Scientists are experimenting with replacing damaged pancreatic cells using lab-grown stem cells, similar to the current breakthrough.
2. Gene Editing (CRISPR Technology)
CRISPR-based tools are being used to correct genetic errors that trigger autoimmune reactions, potentially preventing T1D onset.
3. Immunotherapy
New drugs aim to retrain the immune system to stop attacking pancreatic cells. The FDA recently approved Tzield (teplizumab) — the first drug that can delay the onset of Type 1 diabetes.
4. Artificial Pancreas Systems
Closed-loop insulin pumps paired with continuous glucose monitors (CGMs) automatically adjust insulin doses — simulating natural pancreatic function.
Together, these approaches are inching closer to a world where insulin injections may become obsolete.
ALSO READ: Silent Heart Attacks In Women: Cardiologist Shares Overlooked Warning Signs
The Science Behind Beta Cell Regeneration
Beta cell regeneration involves the restoration or replacement of insulin-producing cells in the pancreas.
In the case study, scientists used induced pluripotent stem cells (iPSCs) — adult cells reprogrammed to behave like embryonic stem cells.
Mechanism of Action
-
Cell reprogramming: Skin or blood cells are turned into iPSCs.
-
Guided growth: iPSCs are cultured into beta-like cells in the lab.
-
Immune evasion: Cells are coated with protective biomaterials to avoid destruction by the immune system.
-
Insulin release: Once implanted, they mimic natural pancreatic function.
This method not only helps restore insulin but also opens doors for organ-specific regeneration in other diseases.
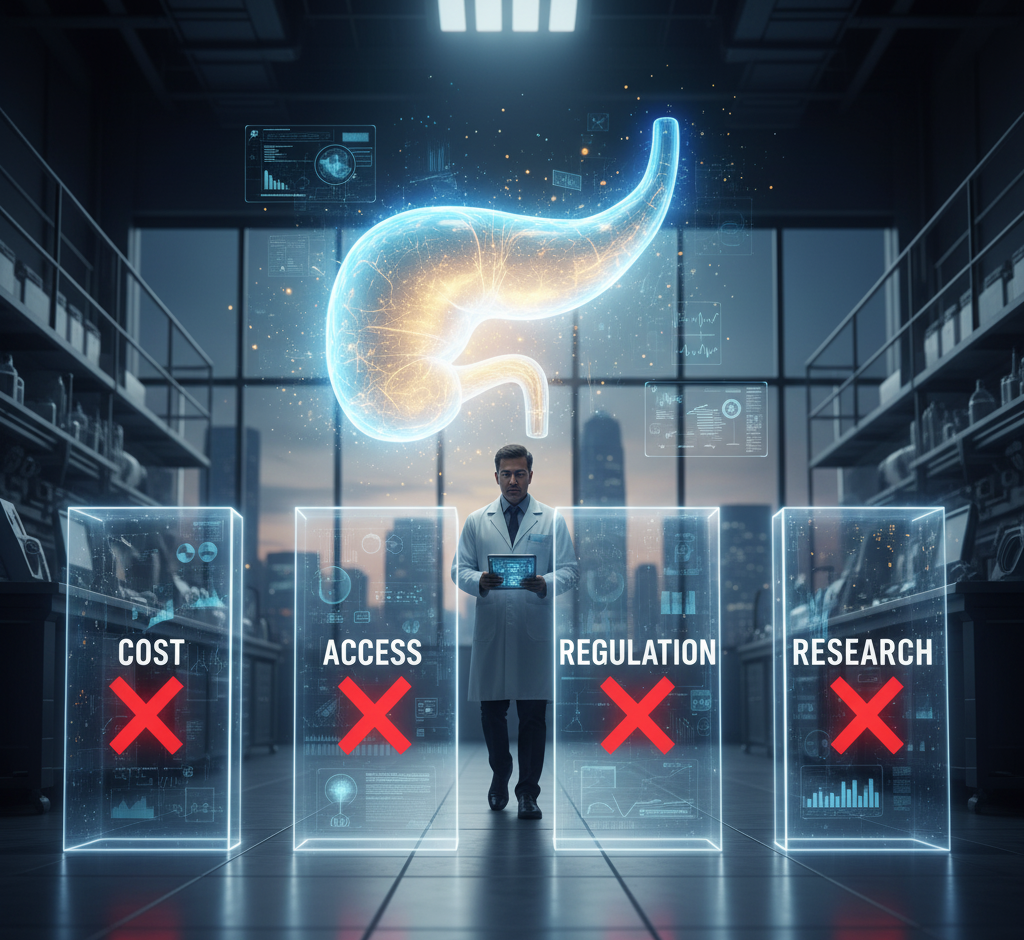
Ethical and Safety Considerations
While the breakthrough is promising, there are ethical and practical questions to consider:
-
Stem cell sourcing: Ensuring ethical derivation and donor consent.
-
Immune rejection: Even encapsulated cells may face immune attack over time.
-
Cancer risk: Uncontrolled cell growth must be prevented through strict regulation.
-
Cost and accessibility: Ensuring affordable access for patients in low- and middle-income countries.
WHO and global health agencies stress that equitable access must be prioritised as regenerative therapies evolve.
Implications for India
India has one of the largest diabetic populations globally, and Type 1 diabetes in children is on the rise.
Leading Indian research centres, such as AIIMS Delhi, IIT Bombay, and Stempeutics Research Bengaluru, are conducting clinical trials on stem cell therapy for diabetes.
The Indian Council of Medical Research (ICMR) has also released guidelines to promote safe and ethical regenerative medicine research.
If this breakthrough becomes mainstream, it could transform India’s diabetes management landscape, particularly for young patients dependent on insulin.
Challenges Ahead
Despite the excitement, several challenges remain before the therapy can become widely available:
-
Long-term safety studies are still ongoing.
-
Large-scale manufacturing of lab-grown beta cells is complex and expensive.
-
Immune protection systems need refinement for durability.
-
Regulatory approvals and standardised clinical protocols must be established.
Nevertheless, researchers are optimistic that with continued trials and investment, a functional cure for Type 1 diabetes may emerge within the next decade.
Lifestyle Still Matters
Even with medical breakthroughs, lifestyle management remains essential.
Healthy nutrition, regular exercise, stress control, and routine glucose monitoring continue to support optimal insulin function and prevent complications.
Quick Tips for Type 1 Diabetics
-
Monitor blood sugar regularly.
-
Choose whole grains, lean proteins, and low-GI foods.
-
Stay hydrated and avoid sugary beverages.
-
Manage stress through yoga and mindfulness.
-
Follow up with an endocrinologist every 3–6 months.
Conclusion
The case of a patient producing his own insulin represents a historic milestone in diabetes research.
It demonstrates the immense potential of regenerative medicine — not just to manage diseases, but to truly heal them.
While it’s too early to declare a complete cure, this breakthrough provides real hope that millions living with Type 1 diabetes could one day live insulin-free lives.
As clinical trials expand globally, India too is poised to play a key role in making this scientific dream a medical reality.
Quickobook Call to Action
Managing Type 1 diabetes or interested in new treatment options?
Book an appointment with an endocrinologist or diabetologist today on Quickobook.com.
Get expert advice on regenerative therapies, advanced glucose monitoring, and insulin management — all in one trusted healthcare platform.
Disclaimer
This article is for educational purposes only and does not substitute for medical advice. Always consult a certified endocrinologist before considering any treatment or clinical trial participation.
50 FAQs About Type 1 Diabetes and Regenerative Medicine
Q1. What is Type 1 diabetes?
An autoimmune condition where the body destroys insulin-producing beta cells in the pancreas.
Q2. What makes this case special?
It’s the first time a long-term diabetic began producing insulin naturally again after stem cell therapy.
Q3. What is regenerative medicine?
A field of medicine that restores or replaces damaged tissues using stem cells and advanced biotechnology.
Q4. How does the therapy work?
Stem cells are converted into insulin-producing cells and implanted to restore pancreas function.
Q5. Is this a permanent cure?
It’s too early to call it a cure, but results are very promising.
Q6. When will it be available in India?
Likely within 5–10 years after successful clinical trials and approvals.
Q7. Can everyone with Type 1 diabetes benefit?
Potentially, but therapy suitability depends on age, immune health, and other factors.
Q8. What is the cost of current trials?
Costs are high now but expected to decrease with large-scale production.
Q9. Is stem cell therapy safe?
So far, early trials show good safety, but long-term data is still needed.
Q10. Does this treatment replace insulin injections completely?
In some patients, yes — though others may still need reduced doses.
Q11. What are beta cells?
Cells in the pancreas that produce insulin.
Q12. Can beta cells grow back naturally?
Not easily — which is why regenerative therapy is groundbreaking.
Q13. What is C-peptide testing?
A blood test that measures the body’s insulin production ability.
Q14. Does diet play a role after therapy?
Yes, healthy diet and exercise remain crucial.
Q15. What’s the difference between Type 1 and Type 2 diabetes?
Type 1 is autoimmune; Type 2 is often lifestyle-related.
Q16. Can gene editing cure diabetes?
Research using CRISPR is ongoing, with promising results.
Q17. How common is Type 1 diabetes in India?
Around 1.5 million people live with it, with rising incidence in children.
Q18. What are the side effects of stem cell therapy?
Minor pain, inflammation, or immune rejection in rare cases.
Q19. What is the lifespan of implanted cells?
Studies show they can function for years, possibly longer with upgrades.
Q20. Can regenerative medicine help other diseases?
Yes, in conditions like heart failure, Parkinson’s, and spinal injury.
Q21. Who can donate stem cells?
Donors must undergo medical screening; some therapies use patient-derived cells.
Q22. Is insulin still needed after therapy?
Some patients achieve full insulin independence; others require less.
Q23. Can children undergo this therapy?
Trials are currently focused on adults, but pediatric studies are planned.
Q24. How are immune attacks prevented?
Through encapsulation and immune-suppressing technology.
Q25. What’s the global impact of this breakthrough?
It may redefine diabetes treatment for future generations.
Q26. Is this therapy approved yet?
Still in advanced clinical trial stages.
Q27. Who developed it?
Researchers at Vertex Pharmaceuticals in collaboration with leading diabetes institutes.
Q28. Can stem cells be made from my blood?
Yes, via induced pluripotent stem cell (iPSC) technology.
Q29. How long does treatment take?
Several months, including preparation and recovery.
Q30. Does it work for Type 2 diabetes too?
Currently designed for Type 1, but research for Type 2 is ongoing.
Q31. Are there risks of cancer from stem cells?
Minimal under strict lab protocols and controlled implantation.
Q32. Is this therapy painful?
Minimally invasive; performed under local or general anaesthesia.
Q33. Can the pancreas heal naturally?
Limited self-repair occurs, but not enough to restore full insulin production.
Q34. How is this monitored post-treatment?
Regular blood glucose, C-peptide, and HbA1c testing.
Q35. What role does Quickobook play?
Quickobook connects patients with endocrinologists and advanced diabetes care centres.
Q36. Is fasting blood sugar still needed after therapy?
Yes, regular monitoring remains vital.
Q37. Can diet alone cure Type 1 diabetes?
No, it helps manage symptoms but doesn’t regenerate beta cells.
Q38. Is insulin-free diabetes management possible soon?
Yes, if ongoing trials continue showing success.
Q39. What is Tzield?
An FDA-approved drug that delays Type 1 diabetes onset.
Q40. What are clinical trials Phase 1–3?
Sequential testing stages to ensure safety and effectiveness.
Q41. Is regenerative medicine available in India?
Yes, but currently limited to research and approved trials.
Q42. What’s the role of the immune system in diabetes?
It mistakenly destroys pancreatic beta cells.
Q43. How can I join a trial?
Check with authorized research centres or through Quickobook’s medical partners.
Q44. Are results permanent?
Still under evaluation, but early data is encouraging.
Q45. What are the success rates so far?
Many patients show partial to full insulin restoration.
Q46. Does yoga or lifestyle help post-treatment?
Yes, reduces stress and improves metabolism.
Q47. What’s next in diabetes research?
Combining gene editing, stem cells, and smart devices.
Q48. How can families support Type 1 diabetics?
By ensuring emotional support, healthy diet, and regular follow-ups.
Q49. Can AI assist in diabetes care?
Yes, AI-based glucose tracking and predictive alerts are emerging tools.
Q50. What’s the future of Type 1 diabetes treatment?
A cure may finally be within reach — thanks to regenerative medicine and scientific innovation.








Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment