Introduction: When Alcohol Starts Hurting Your Liver
The liver is one of the body’s most hardworking organs—responsible for detoxifying harmful substances, digesting fats, and storing nutrients. But when alcohol is consumed regularly and in excess, it begins to damage liver cells.
This early stage of liver damage is called Alcoholic Fatty Liver Disease (AFLD), and it is far more common than many realize. In India, alcohol-related liver disease contributes to over 30% of chronic liver cases, often affecting adults between 25–50 years.
The good news? Alcoholic fatty liver is reversible if diagnosed early and managed through abstinence, medical guidance, and a healthy liver diet.
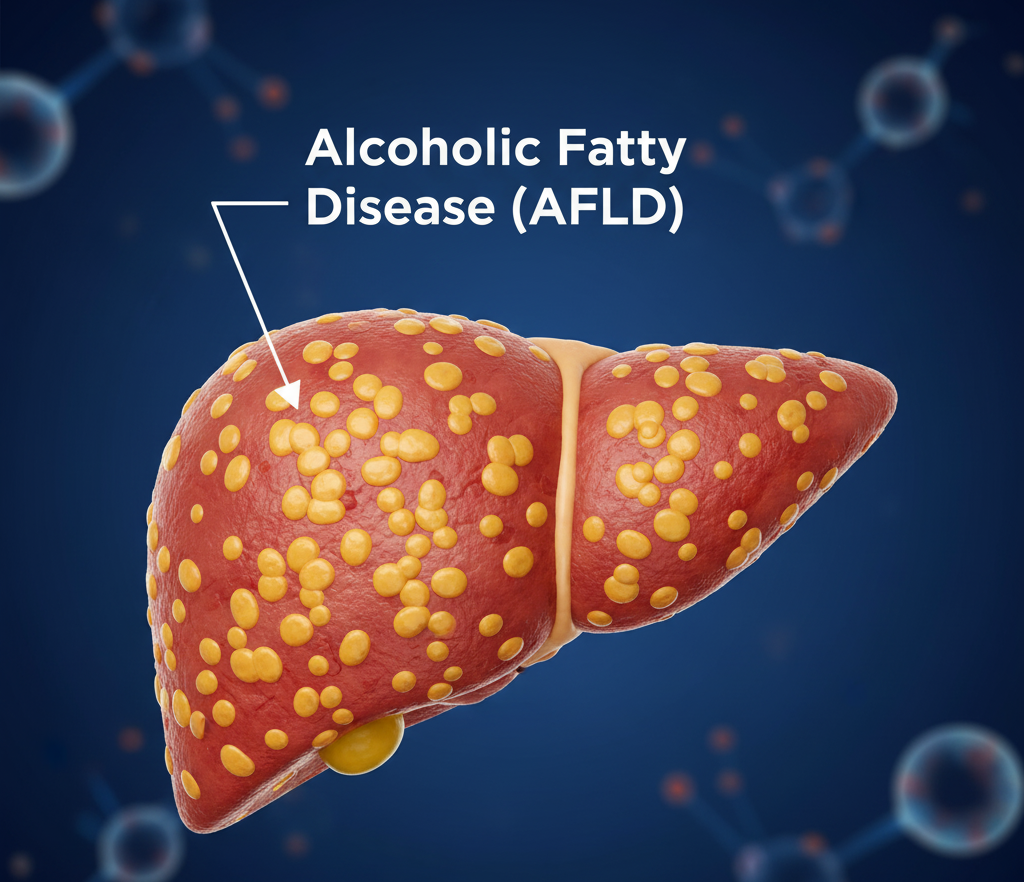
What Is Alcoholic Fatty Liver Disease (AFLD)?
AFLD occurs when fat accumulates inside the liver due to excessive alcohol consumption. The liver normally breaks down alcohol, but over time, the toxins generated can inflame and injure liver cells.
If the damage continues unchecked, AFLD may progress to more serious conditions such as:
-
Alcoholic Hepatitis – inflammation and swelling of the liver.
-
Alcoholic Cirrhosis – irreversible scarring of liver tissue.
How Alcohol Affects the Liver
When alcohol enters the bloodstream, the liver works to metabolize it. During this process, harmful byproducts like acetaldehyde are produced, damaging liver cells and reducing fat metabolism.
As a result, fat starts accumulating in liver cells—marking the first stage of alcoholic liver disease. With continued drinking, this fat buildup triggers inflammation and eventually scarring.
Stages of Alcohol-Related Liver Disease
-
Alcoholic Fatty Liver (Steatosis): Reversible stage with fat deposits in liver.
-
Alcoholic Hepatitis: Inflammation, pain, and liver dysfunction.
-
Alcoholic Cirrhosis: Severe, irreversible scarring and liver failure.
The earlier you intervene, the higher the chances of recovery.
Symptoms of Alcoholic Fatty Liver Disease
In its early stages, AFLD often shows no noticeable symptoms. As it progresses, signs may include:
-
Constant fatigue or weakness
-
Loss of appetite
-
Mild abdominal discomfort or fullness
-
Nausea or vomiting
-
Yellowing of eyes or skin (jaundice)
-
Swollen legs or abdomen (edema/ascites)
-
Weight loss and muscle thinning
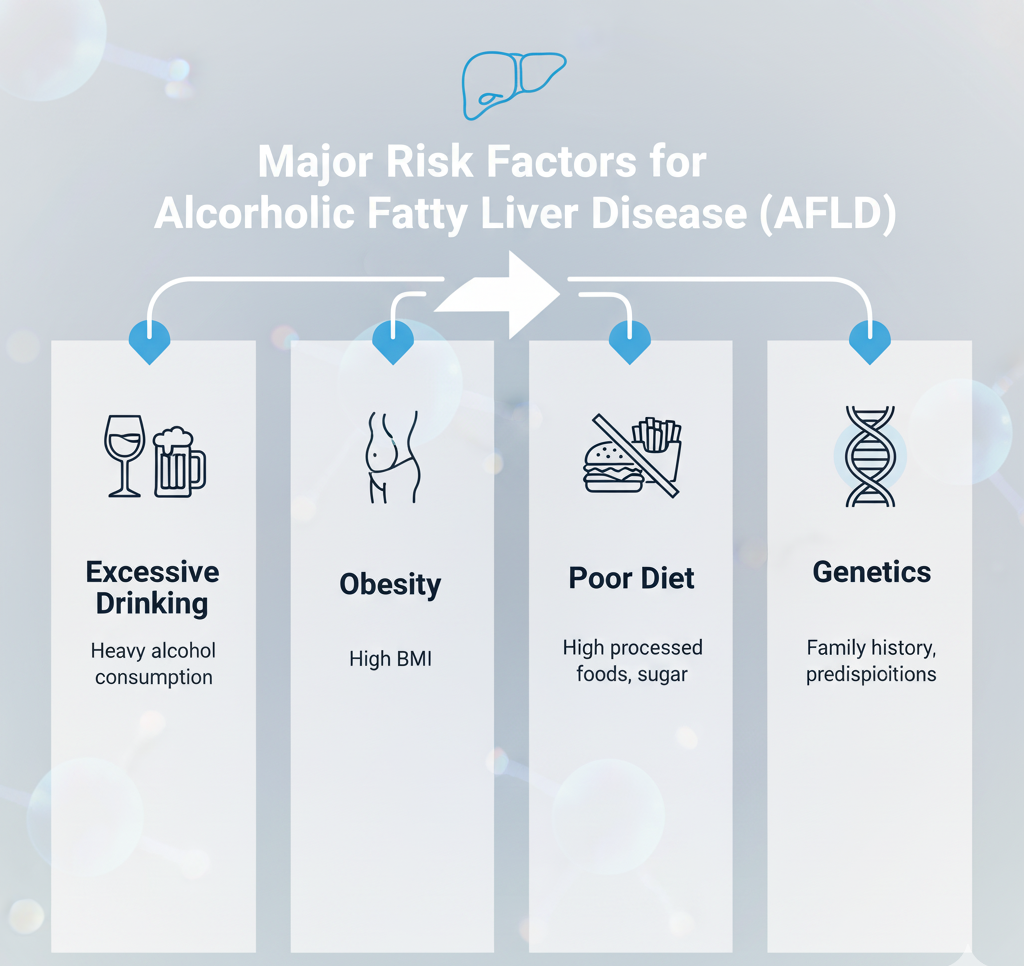
Causes and Risk Factors
-
Regular and heavy alcohol use (even 2–3 drinks daily over years)
-
Poor nutrition or protein deficiency
-
Obesity and high-fat diet
-
Genetic predisposition
-
Hepatitis C infection
-
Female gender (women’s livers process alcohol more slowly)
Diagnosis of AFLD
Doctors diagnose AFLD through physical exams, blood tests, and imaging.
Common diagnostic tests include:
-
Liver Function Tests (LFTs) – elevated liver enzymes indicate inflammation.
-
Ultrasound Abdomen – shows fatty changes in the liver.
-
CT/MRI Scan – detailed view of liver texture.
-
FibroScan – measures liver stiffness and fibrosis.
-
Liver Biopsy – confirms diagnosis if needed.
Treatment and Recovery
The most important treatment for alcoholic fatty liver is complete abstinence from alcohol. Stopping alcohol allows the liver to heal and regenerate new cells.
Treatment steps include:
-
Quit alcohol completely.
-
Seek help through de-addiction programs or counseling if needed.
-
-
Follow a healthy liver diet.
-
Eat nutrient-rich meals with fruits, vegetables, and whole grains.
-
-
Medications (as advised by doctor).
-
Supplements like vitamin E, B-complex, or antioxidants may help recovery.
-
-
Monitor liver health.
-
Regular check-ups and liver tests every 3–6 months.
-
If diagnosed early, AFLD can completely reverse within 6–8 weeks of alcohol abstinence.
Healthy Liver Diet: Supporting Recovery Naturally
A well-balanced diet plays a vital role in liver healing.
Foods to include:
-
Fresh fruits: papaya, apple, berries, oranges.
-
Vegetables: spinach, broccoli, beets, carrots.
-
Whole grains and legumes.
-
Lean proteins: fish, eggs, tofu, and lentils.
-
Healthy fats: olive oil, nuts, and seeds.
-
Plenty of water and herbal teas.
Foods to avoid:
-
Fried and processed foods.
-
Sugary drinks and refined carbs.
-
Red meat and saturated fats.
-
Alcohol (strictly prohibited).
Pro tip: Eat smaller, frequent meals and avoid skipping breakfast.
Complications of Untreated AFLD
Ignoring alcoholic fatty liver can lead to severe health consequences, including:
-
Cirrhosis – irreversible scarring.
-
Liver failure – inability to filter toxins.
-
Ascites – fluid accumulation in the abdomen.
-
Hepatic encephalopathy – confusion due to toxin buildup.
-
Liver cancer.

When to See a Doctor
Seek medical help if you notice:
-
Fatigue or yellowing of eyes
-
Nausea or poor appetite
-
Swollen abdomen or legs
-
Pain in the upper right side of the stomach
Quickobook helps you book appointments with hepatologists or gastroenterologists for early diagnosis and treatment.
Prevention Tips for Alcoholic Fatty Liver Disease
-
Limit or completely avoid alcohol.
-
Eat a nutrient-rich, liver-friendly diet.
-
Exercise regularly.
-
Stay hydrated.
-
Manage diabetes and obesity.
-
Get routine liver function tests every 6–12 months.
Conclusion
Alcoholic Fatty Liver Disease (AFLD) is an early warning that your liver is under stress. The condition is reversible if addressed in time—by quitting alcohol, eating right, and following medical advice.
Your liver has incredible healing power; all it needs is care, consistency, and commitment. If you or someone you know struggles with alcohol-related liver problems, seek professional help immediately.
Quickobook CTA
Book a consultation with a hepatologist or liver specialist on Quickobook for AFLD screening and treatment.
Visit Quickobook.com for trusted doctors, transparent fees, and online appointment booking.
50 FAQs: Alcoholic Fatty Liver Disease (AFLD)
Q1. What is alcoholic fatty liver disease?
It’s the first stage of alcohol-related liver damage where fat builds up inside liver cells.
Q2. Can alcoholic fatty liver be reversed?
Yes, if you stop drinking and follow a healthy liver diet.
Q3. How long does it take to heal?
Usually within 6–8 weeks of complete alcohol abstinence.
Q4. What are the early symptoms?
Fatigue, loss of appetite, mild abdominal discomfort.
Q5. Can it occur in occasional drinkers?
Yes, regular small amounts can still cause damage over time.
Q6. Is alcoholic fatty liver painful?
Usually mild discomfort or heaviness in the upper abdomen.
Q7. What foods help repair the liver?
Leafy greens, fruits, olive oil, and whole grains.
Q8. Can vitamins help the liver heal?
Yes, vitamin B complex and E may support recovery.
Q9. What is alcoholic hepatitis?
An advanced stage of AFLD with liver inflammation.
Q10. Can cirrhosis be reversed?
No, it’s irreversible; early detection is key.
Q11. How much alcohol is too much?
More than 2 drinks daily for men, 1 for women increases risk.
Q12. Can women get alcoholic fatty liver faster?
Yes, women’s bodies process alcohol less efficiently.
Q13. What tests detect AFLD?
LFT, ultrasound, CT scan, and FibroScan.
Q14. Can stress worsen liver health?
Yes, it affects hormones and metabolism.
Q15. Is it okay to drink “occasionally” after recovery?
No, even small amounts can trigger relapse.
Q16. Can coffee protect the liver?
Yes, moderate coffee intake may reduce liver inflammation.
Q17. What are signs of severe liver damage?
Jaundice, swelling, confusion, and dark urine.
Q18. Can alcoholic liver disease cause cancer?
Yes, long-term inflammation may lead to liver cancer.
Q19. How can I detox my liver naturally?
By quitting alcohol, staying hydrated, and eating clean foods.
Q20. What happens if AFLD is untreated?
It can progress to cirrhosis and liver failure.
Q21. Can yoga help liver health?
Yes, yoga improves blood flow and stress control.
Q22. Can alcohol affect other organs too?
Yes, it harms the pancreas, heart, and brain.
Q23. What is the difference between AFLD and NAFLD?
AFLD is alcohol-induced; NAFLD occurs without alcohol.
Q24. Is fatty liver hereditary?
Genetics can increase susceptibility.
Q25. Can dehydration harm the liver?
Yes, hydration is essential for toxin removal.
Q26. What are safe alternatives to alcohol?
Mocktails, coconut water, herbal teas.
Q27. Can smoking affect liver health?
Yes, smoking worsens oxidative stress.
Q28. Is liver pain common in AFLD?
Usually mild unless inflammation is severe.
Q29. Can fatty liver cause nausea?
Yes, due to impaired digestion.
Q30. What’s the role of protein in liver recovery?
Lean protein helps regenerate cells.
Q31. Should I avoid medicines with alcohol content?
Yes, always check labels and consult your doctor.
Q32. Can obesity worsen AFLD?
Yes, it accelerates liver fat accumulation.
Q33. What is a healthy liver diet?
A balanced diet rich in antioxidants, fiber, and omega-3 fats.
Q34. Can fatty liver cause sleep problems?
Yes, due to metabolic and hormonal imbalance.
Q35. How much water should I drink daily?
At least 2–3 liters, depending on your body weight.
Q36. Are supplements like milk thistle useful?
They may help but only under medical supervision.
Q37. Can skipping meals worsen liver issues?
Yes, it slows metabolism and increases fat storage.
Q38. How can I prevent relapse after recovery?
Avoid alcohol entirely and continue regular check-ups.
Q39. Can alcohol withdrawal cause side effects?
Yes, seek medical support for safe detox.
Q40. How does AFLD affect digestion?
It impairs fat metabolism and bile production.
Q41. What are signs of cirrhosis?
Jaundice, bleeding, confusion, and abdominal swelling.
Q42. Can fatty liver cause body odor?
Not directly, but poor detox function may contribute.
Q43. What is the best exercise for liver health?
Brisk walking, yoga, and swimming.
Q44. Can fatty liver cause acidity?
Sometimes, due to sluggish digestion.
Q45. Is it okay to take painkillers with liver disease?
Only under medical supervision.
Q46. Can fatty liver lead to weight loss?
Yes, in advanced stages due to poor metabolism.
Q47. What is hepatic encephalopathy?
Brain dysfunction from severe liver failure.
Q48. How to check if my liver is healing?
Monitor enzyme levels and imaging results.
Q49. How often should I see a doctor?
Every 3–6 months for follow-up.
Q50. Where can I book a liver health check-up?
Visit Quickobook.com to book hepatologists or gastroenterologists online.







Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment