Health
Introduction
Lionel Messi is known across the world for his football skills, discipline, and consistency. From a young boy with a growth hormone deficiency to one of the greatest footballers of all time, his journey teaches us powerful life lessons. These lessons go beyond sports. They apply equally to health, self-care, and access to the right support at the right time.
In India, millions of people struggle not because treatment does not exist, but because healthcare access is delayed or confusing. This is where Quickobook steps in. Just like Messi focuses on preparation, routine, and the right guidance, Quickobook focuses on connecting patients to the right doctors using technology in healthcare.
This blog explores how the values behind Lionel Messi align with the mission of Quickobook, and why these lessons matter for everyday health decisions.
Why Compare Lionel Messi and Quickobook?
At first glance, football and healthcare may seem unrelated. But if we look deeper, both rely on preparation, teamwork, discipline, and timely decisions.
Messi succeeded because:
He received the right medical care early
He followed strict routines
He trusted experts
He stayed consistent
Quickobook works on the same principles:
Early access to doctors
Easy appointment booking
Trust and transparency
Consistent, patient-first care
Both show us that success, whether in sports or health, depends on access, discipline, and the right system.
Lionel Messi’s Health Journey: A Lesson in Early Medical Care
As a child, Lionel Messi was diagnosed with growth hormone deficiency. This condition affects height and physical development. Without treatment, his football career might never have started.
His family ensured:
Early diagnosis
Specialist consultation
Long-term treatment
Consistent follow-ups
This story highlights one clear truth. Timely healthcare access can change lives.
In India, many children and adults face delays in diagnosis due to lack of awareness or difficulty finding doctors. Platforms like Quickobook help reduce these delays by making doctor discovery simple and fast.
Healthcare Access in India: The Real Challenge
India has skilled doctors and advanced hospitals. The real problem is not availability, but access.
Common issues include:
Long waiting times
Confusion about which doctor to consult
Distance to clinics
Lack of digital booking options
Missed follow-ups
Just like a footballer cannot perform without the right support team, patients struggle without a clear healthcare pathway.
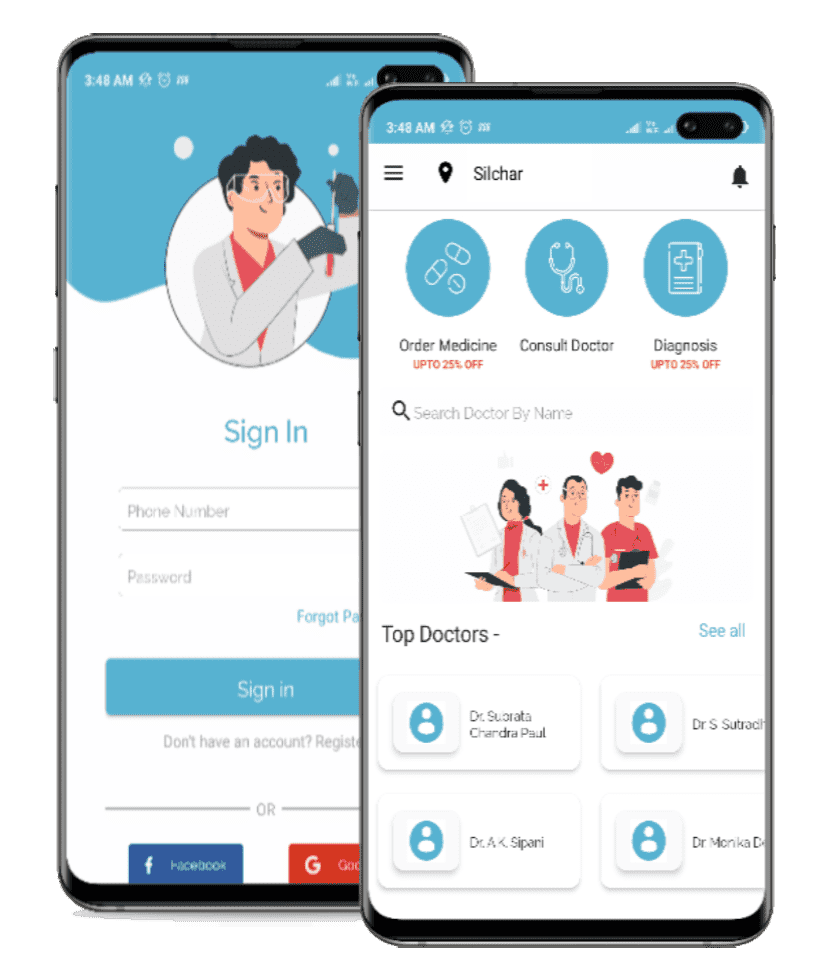
Quickobook: Simplifying Healthcare with Technology
Quickobook is designed to solve every day healthcare problems using technology in healthcare. It acts as a bridge between patients and doctors.
Key benefits include:
Easy online doctor search
Appointment booking in minutes
Verified doctor profiles
Reduced waiting time
Better follow-up care
For patients, this means less stress. For doctors, it means better patient management. This balance reflects the teamwork seen in professional sports like football.
Discipline and Routine: Messi’s Biggest Strength
Lionel Messi is not just talented. He is disciplined.
His routine includes:
Regular health check-ups
Fitness monitoring
Injury prevention
Mental health focus
Rest and recovery
These habits are equally important for non-athletes. Regular health check-ups help detect problems early. Quickobook encourages preventive healthcare by making routine doctor visits easier to schedule.
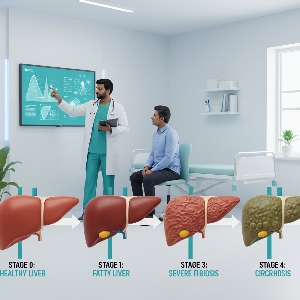
Preventive Healthcare: What Messi Teaches Every Indian Family
Preventive care means seeing a doctor before a problem becomes serious. Messi’s career longevity proves its value.
Preventive healthcare includes:
Annual health check-ups
Monitoring blood pressure and sugar
Early screening tests
Vaccinations
Lifestyle counselling
Quickobook supports this approach by helping families find general physicians and specialists nearby, without long delays.
Technology in Healthcare: Changing How India Sees Doctors
Just like modern football uses data, fitness tracking, and video analysis, modern healthcare uses digital tools.
Technology in healthcare helps with:
Online appointment booking
Teleconsultation
Digital health records
Reminders for follow-ups
Better doctor-patient communication
Quickobook uses these tools to make healthcare less complicated and more human.
Mental Health: An Often Ignored Lesson from Sports
Top athletes work with psychologists to manage stress, pressure, and expectations. Messi is no exception.
In daily life, mental health is often ignored due to stigma or lack of access. Quickobook helps people find mental health professionals discreetly and easily, promoting balanced well-being.
Why Trust Matters in Both Football and Healthcare
Messi trusts his coaches, doctors, and physiotherapists. This trust allows him to focus on performance.
Similarly, patients need:
Verified doctors
Transparent information
Honest reviews
Clear communication
Quickobook builds trust by listing verified doctors and patient feedback, helping users make informed choices.
From Stadiums to Clinics: The Same Winning Formula
The same formula that builds champions also builds healthy communities:
Early action
Expert guidance
Consistency
Discipline
Right use of technology
Quickobook applies this formula to Indian healthcare, inspired by stories like Lionel Messi’s.
When to See a Doctor: Don’t Delay
You should book a doctor appointment if you have:
Persistent pain
Fever lasting more than 3 days
Sudden weight loss
Breathing difficulty
Mental stress or anxiety
Chronic lifestyle conditions
Early consultation saves money, time, and health.
Risks of Delayed Healthcare
Ignoring symptoms can lead to:
Complications
Longer treatment
Higher medical costs
Hospitalisation
Permanent damage
Messi’s early treatment prevented long-term problems. The same principle applies to everyone.
Lifestyle Lessons from Lionel Messi
Messi’s lifestyle focuses on balance:
Healthy diet
Regular exercise
Proper sleep
Stress management
Doctors available on Quickobook can help guide patients toward healthier routines suited to Indian lifestyles.
Conclusion
Lionel Messi’s life proves that talent alone is not enough. Timely medical care, discipline, and access to experts play a key role in long-term success. In the same way, Quickobook is changing how Indians approach healthcare by improving healthcare access through technology in healthcare.
Whether you are managing a condition or simply staying healthy, the right doctor at the right time can make all the difference.
Quickobook Call to Action
Book verified doctors near you
Avoid long waiting lines
Manage your health digitally
Take control of your well-being today with Quickobook
Frequently Asked Questions
Q1. Who is Lionel Messi?
A. Lionel Messi is a world-famous footballer known for skill, discipline, and consistency.
Q2. What health issue did Messi face as a child?
A. He had growth hormone deficiency, treated with early medical care.
Q3. Why is Messi’s story relevant to healthcare?
A. It shows how early access to treatment can change lives.
Q4. What is Quickobook?
A. Quickobook is a digital platform to book doctor appointments easily.
Q5. How does Quickobook improve healthcare access?
A. It connects patients with doctors quickly using technology.
Q6. Is Quickobook available in India?
A. Yes, it is designed for Indian healthcare needs.
Q7. Can I book general physicians on Quickobook?
A. Yes, you can book general and specialist doctors.
Q8. Does Quickobook reduce waiting time?
A. Yes, it helps schedule appointments in advance.
Q9. What is preventive healthcare?
A. It means seeing doctors early to avoid serious illness.
Q10. Why is preventive care important?
A. It reduces complications and healthcare costs.
Q11. How does technology help healthcare?
A. It simplifies booking, follow-ups, and communication.
Q12. Can Quickobook help with mental health?
A. Yes, mental health professionals are available.
Q13. Is Quickobook suitable for families?
A. Yes, it supports healthcare for all age groups.
Q14. Does Messi focus on mental fitness?
A. Yes, mental strength is key in professional sports.
Q15. Can regular check-ups prevent disease?
A. Yes, many conditions are manageable if detected early.
Q16. Is online doctor booking safe?
A. Yes, when using verified platforms like Quickobook.
Q17. How often should adults see a doctor?
A. At least once a year for routine check-ups.
Q18. What conditions need immediate consultation?
A. Chest pain, breathlessness, and severe fever.
Q19. Can lifestyle changes improve health?
A. Yes, diet, exercise, and sleep make a big difference.
Q20. Does Quickobook support follow-ups?
A. Yes, it helps maintain continuity of care.
Q21. Why is trust important in healthcare?
A. It improves treatment outcomes and patient comfort.
Q22. How does Quickobook verify doctors?
A. Through qualification and registration checks.
Q23. Can rural patients use Quickobook?
A. Yes, availability depends on nearby doctors.
Q24. Does Quickobook offer teleconsultation?
A. Many doctors provide online consultations.
Q25. What lesson does Messi teach about discipline?
A. Consistency leads to long-term success.
Q26. Is delayed treatment risky?
A. Yes, it can worsen health conditions.
Q27. Can Quickobook help with chronic diseases?
A. Yes, it helps manage regular doctor visits.
Q28. Why is early diagnosis important?
A. It prevents complications and improves outcomes.
Q29. Does Quickobook save time?
A. Yes, by reducing clinic waiting hours.
Q30. Is healthcare access a problem in India?
A. Yes, especially due to delays and lack of awareness.
Q31. Can technology replace doctors?
A. No, it supports doctors, not replaces them.
Q32. Does Messi follow a strict routine?
A. Yes, for fitness and injury prevention.
Q33. Can routine help non-athletes?
A. Yes, routines improve overall health.
Q34. Are regular tests necessary?
A. Yes, for early detection of health issues.
Q35. Does Quickobook list specialists?
A. Yes, across multiple medical fields.
Q36. Is Quickobook user-friendly?
A. Yes, it is designed for easy use.
Q37. Can older adults use Quickobook?
A. Yes, with simple booking options.
Q38. What role does awareness play in health?
A. It helps people seek care early.
Q39. Does Messi’s success rely only on talent?
A. No, it also relies on medical and professional support.
Q40. Can Quickobook help in emergencies?
A. It helps find doctors quickly, but emergencies need hospitals.
Q41. Is digital healthcare the future?
A. Yes, it improves efficiency and access.
Q42. Does Quickobook show doctor reviews?
A. Yes, patient feedback is available.
Q43. Can booking online reduce stress?
A. Yes, it avoids uncertainty and delays.
Q44. Are check-ups expensive?
A. Costs vary, but prevention saves money long-term.
Q45. Can lifestyle counselling help?
A. Yes, doctors can guide healthy habits.
Q46. Does Quickobook support preventive care?
A. Yes, by encouraging regular visits.
Q47. What is the biggest healthcare lesson from Messi?
A. Never delay proper medical care.
Q48. Is healthcare a team effort?
A. Yes, between patient, doctor, and system.
Q49. Can one platform improve healthcare habits?
A. Yes, by making access easy and reliable.
Q50. How can I start using Quickobook?
A. By booking your first doctor appointment online.
Introduction
Lionel Messi is known across the world for his football skills, discipline, and consistency. From a young boy with a growth hormone deficiency to one of the greatest footballers of all time, his journey teaches us powerful life lessons. These lessons go beyond sports. They apply equally to health, self-care, and access to the right support at the right time.
In India, millions of people struggle not because treatment does not exist, but because healthcare access is delayed or confusing. This is where Quickobook steps in. Just like Messi focuses on preparation, routine, and the right guidance, Quickobook focuses on connecting patients to the right doctors using technology in healthcare.
This blog explores how the values behind Lionel Messi align with the mission of Quickobook, and why these lessons matter for everyday health decisions.
Why Compare Lionel Messi and Quickobook?
At first glance, football and healthcare may seem unrelated. But if we look deeper, both rely on preparation, teamwork, discipline, and timely decisions.
Messi succeeded because:
He received the right medical care early
He followed strict routines
He trusted experts
He stayed consistent
Quickobook works on the same principles:
Early access to doctors
Easy appointment booking
Trust and transparency
Consistent, patient-first care
Both show us that success, whether in sports or health, depends on access, discipline, and the right system.
Lionel Messi’s Health Journey: A Lesson in Early Medical Care
As a child, Lionel Messi was diagnosed with growth hormone deficiency. This condition affects height and physical development. Without treatment, his football career might never have started.
His family ensured:
Early diagnosis
Specialist consultation
Long-term treatment
Consistent follow-ups
This story highlights one clear truth. Timely healthcare access can change lives.
In India, many children and adults face delays in diagnosis due to lack of awareness or difficulty finding doctors. Platforms like Quickobook help reduce these delays by making doctor discovery simple and fast.
Healthcare Access in India: The Real Challenge
India has skilled doctors and advanced hospitals. The real problem is not availability, but access.
Common issues include:
Long waiting times
Confusion about which doctor to consult
Distance to clinics
Lack of digital booking options
Missed follow-ups
Just like a footballer cannot perform without the right support team, patients struggle without a clear healthcare pathway.
Quickobook: Simplifying Healthcare with Technology
Quickobook is designed to solve every day healthcare problems using technology in healthcare. It acts as a bridge between patients and doctors.
Key benefits include:
Easy online doctor search
Appointment booking in minutes
Verified doctor profiles
Reduced waiting time
Better follow-up care
For patients, this means less stress. For doctors, it means better patient management. This balance reflects the teamwork seen in professional sports like football.
Discipline and Routine: Messi’s Biggest Strength
Lionel Messi is not just talented. He is disciplined.
His routine includes:
Regular health check-ups
Fitness monitoring
Injury prevention
Mental health focus
Rest and recovery
These habits are equally important for non-athletes. Regular health check-ups help detect problems early. Quickobook encourages preventive healthcare by making routine doctor visits easier to schedule.
Preventive Healthcare: What Messi Teaches Every Indian Family
Preventive care means seeing a doctor before a problem becomes serious. Messi’s career longevity proves its value.
Preventive healthcare includes:
Annual health check-ups
Monitoring blood pressure and sugar
Early screening tests
Vaccinations
Lifestyle counselling
Quickobook supports this approach by helping families find general physicians and specialists nearby, without long delays.
Technology in Healthcare: Changing How India Sees Doctors
Just like modern football uses data, fitness tracking, and video analysis, modern healthcare uses digital tools.
Technology in healthcare helps with:
Online appointment booking
Teleconsultation
Digital health records
Reminders for follow-ups
Better doctor-patient communication
Quickobook uses these tools to make healthcare less complicated and more human.
Mental Health: An Often Ignored Lesson from Sports
Top athletes work with psychologists to manage stress, pressure, and expectations. Messi is no exception.
In daily life, mental health is often ignored due to stigma or lack of access. Quickobook helps people find mental health professionals discreetly and easily, promoting balanced well-being.
Why Trust Matters in Both Football and Healthcare
Messi trusts his coaches, doctors, and physiotherapists. This trust allows him to focus on performance.
Similarly, patients need:
Verified doctors
Transparent information
Honest reviews
Clear communication
Quickobook builds trust by listing verified doctors and patient feedback, helping users make informed choices.
From Stadiums to Clinics: The Same Winning Formula
The same formula that builds champions also builds healthy communities:
Early action
Expert guidance
Consistency
Discipline
Right use of technology
Quickobook applies this formula to Indian healthcare, inspired by stories like Lionel Messi’s.
When to See a Doctor: Don’t Delay
You should book a doctor appointment if you have:
Persistent pain
Fever lasting more than 3 days
Sudden weight loss
Breathing difficulty
Mental stress or anxiety
Chronic lifestyle conditions
Early consultation saves money, time, and health.
Risks of Delayed Healthcare
Ignoring symptoms can lead to:
Complications
Longer treatment
Higher medical costs
Hospitalisation
Permanent damage
Messi’s early treatment prevented long-term problems. The same principle applies to everyone.
Lifestyle Lessons from Lionel Messi
Messi’s lifestyle focuses on balance:
Healthy diet
Regular exercise
Proper sleep
Stress management
Doctors available on Quickobook can help guide patients toward healthier routines suited to Indian lifestyles.
Conclusion
Lionel Messi’s life proves that talent alone is not enough. Timely medical care, discipline, and access to experts play a key role in long-term success. In the same way, Quickobook is changing how Indians approach healthcare by improving healthcare access through technology in healthcare.
Whether you are managing a condition or simply staying healthy, the right doctor at the right time can make all the difference.
Quickobook Call to Action
Book verified doctors near you
Avoid long waiting lines
Manage your health digitally
Take control of your well-being today with Quickobook
Frequently Asked Questions
Q1. Who is Lionel Messi?
A. Lionel Messi is a world-famous footballer known for skill, discipline, and consistency.
Q2. What health issue did Messi face as a child?
A. He had growth hormone deficiency, treated with early medical care.
Q3. Why is Messi’s story relevant to healthcare?
A. It shows how early access to treatment can change lives.
Q4. What is Quickobook?
A. Quickobook is a digital platform to book doctor appointments easily.
Q5. How does Quickobook improve healthcare access?
A. It connects patients with doctors quickly using technology.
Q6. Is Quickobook available in India?
A. Yes, it is designed for Indian healthcare needs.
Q7. Can I book general physicians on Quickobook?
A. Yes, you can book general and specialist doctors.
Q8. Does Quickobook reduce waiting time?
A. Yes, it helps schedule appointments in advance.
Q9. What is preventive healthcare?
A. It means seeing doctors early to avoid serious illness.
Q10. Why is preventive care important?
A. It reduces complications and healthcare costs.
Q11. How does technology help healthcare?
A. It simplifies booking, follow-ups, and communication.
Q12. Can Quickobook help with mental health?
A. Yes, mental health professionals are available.
Q13. Is Quickobook suitable for families?
A. Yes, it supports healthcare for all age groups.
Q14. Does Messi focus on mental fitness?
A. Yes, mental strength is key in professional sports.
Q15. Can regular check-ups prevent disease?
A. Yes, many conditions are manageable if detected early.
Q16. Is online doctor booking safe?
A. Yes, when using verified platforms like Quickobook.
Q17. How often should adults see a doctor?
A. At least once a year for routine check-ups.
Q18. What conditions need immediate consultation?
A. Chest pain, breathlessness, and severe fever.
Q19. Can lifestyle changes improve health?
A. Yes, diet, exercise, and sleep make a big difference.
Q20. Does Quickobook support follow-ups?
A. Yes, it helps maintain continuity of care.
Q21. Why is trust important in healthcare?
A. It improves treatment outcomes and patient comfort.
Q22. How does Quickobook verify doctors?
A. Through qualification and registration checks.
Q23. Can rural patients use Quickobook?
A. Yes, availability depends on nearby doctors.
Q24. Does Quickobook offer teleconsultation?
A. Many doctors provide online consultations.
Q25. What lesson does Messi teach about discipline?
A. Consistency leads to long-term success.
Q26. Is delayed treatment risky?
A. Yes, it can worsen health conditions.
Q27. Can Quickobook help with chronic diseases?
A. Yes, it helps manage regular doctor visits.
Q28. Why is early diagnosis important?
A. It prevents complications and improves outcomes.
Q29. Does Quickobook save time?
A. Yes, by reducing clinic waiting hours.
Q30. Is healthcare access a problem in India?
A. Yes, especially due to delays and lack of awareness.
Q31. Can technology replace doctors?
A. No, it supports doctors, not replaces them.
Q32. Does Messi follow a strict routine?
A. Yes, for fitness and injury prevention.
Q33. Can routine help non-athletes?
A. Yes, routines improve overall health.
Q34. Are regular tests necessary?
A. Yes, for early detection of health issues.
Q35. Does Quickobook list specialists?
A. Yes, across multiple medical fields.
Q36. Is Quickobook user-friendly?
A. Yes, it is designed for easy use.
Q37. Can older adults use Quickobook?
A. Yes, with simple booking options.
Q38. What role does awareness play in health?
A. It helps people seek care early.
Q39. Does Messi’s success rely only on talent?
A. No, it also relies on medical and professional support.
Q40. Can Quickobook help in emergencies?
A. It helps find doctors quickly, but emergencies need hospitals.
Q41. Is digital healthcare the future?
A. Yes, it improves efficiency and access.
Q42. Does Quickobook show doctor reviews?
A. Yes, patient feedback is available.
Q43. Can booking online reduce stress?
A. Yes, it avoids uncertainty and delays.
Q44. Are check-ups expensive?
A. Costs vary, but prevention saves money long-term.
Q45. Can lifestyle counselling help?
A. Yes, doctors can guide healthy habits.
Q46. Does Quickobook support preventive care?
A. Yes, by encouraging regular visits.
Q47. What is the biggest healthcare lesson from Messi?
A. Never delay proper medical care.
Q48. Is healthcare a team effort?
A. Yes, between patient, doctor, and system.
Q49. Can one platform improve healthcare habits?
A. Yes, by making access easy and reliable.
Q50. How can I start using Quickobook?
A. By booking your first doctor appointment online.
Introduction
Lionel Messi is known across the world for his football skills, discipline, and consistency. From a young boy with a growth hormone deficiency to one of the greatest footballers of all time, his journey teaches us powerful life lessons. These lessons go beyond sports. They apply equally to health, self-care, and access to the right support at the right time.
In India, millions of people struggle not because treatment does not exist, but because healthcare access is delayed or confusing. This is where Quickobook steps in. Just like Messi focuses on preparation, routine, and the right guidance, Quickobook focuses on connecting patients to the right doctors using technology in healthcare.
This blog explores how the values behind Lionel Messi align with the mission of Quickobook, and why these lessons matter for everyday health decisions.
Why Compare Lionel Messi and Quickobook?
At first glance, football and healthcare may seem unrelated. But if we look deeper, both rely on preparation, teamwork, discipline, and timely decisions.
Messi succeeded because:
He received the right medical care early
He followed strict routines
He trusted experts
He stayed consistent
Quickobook works on the same principles:
Early access to doctors
Easy appointment booking
Trust and transparency
Consistent, patient-first care
Both show us that success, whether in sports or health, depends on access, discipline, and the right system.
Lionel Messi’s Health Journey: A Lesson in Early Medical Care
As a child, Lionel Messi was diagnosed with growth hormone deficiency. This condition affects height and physical development. Without treatment, his football career might never have started.
His family ensured:
Early diagnosis
Specialist consultation
Long-term treatment
Consistent follow-ups
This story highlights one clear truth. Timely healthcare access can change lives.
In India, many children and adults face delays in diagnosis due to lack of awareness or difficulty finding doctors. Platforms like Quickobook help reduce these delays by making doctor discovery simple and fast.
Healthcare Access in India: The Real Challenge
India has skilled doctors and advanced hospitals. The real problem is not availability, but access.
Common issues include:
Long waiting times
Confusion about which doctor to consult
Distance to clinics
Lack of digital booking options
Missed follow-ups
Just like a footballer cannot perform without the right support team, patients struggle without a clear healthcare pathway.
Quickobook: Simplifying Healthcare with Technology
Quickobook is designed to solve every day healthcare problems using technology in healthcare. It acts as a bridge between patients and doctors.
Key benefits include:
Easy online doctor search
Appointment booking in minutes
Verified doctor profiles
Reduced waiting time
Better follow-up care
For patients, this means less stress. For doctors, it means better patient management. This balance reflects the teamwork seen in professional sports like football.
Discipline and Routine: Messi’s Biggest Strength
Lionel Messi is not just talented. He is disciplined.
His routine includes:
Regular health check-ups
Fitness monitoring
Injury prevention
Mental health focus
Rest and recovery
These habits are equally important for non-athletes. Regular health check-ups help detect problems early. Quickobook encourages preventive healthcare by making routine doctor visits easier to schedule.
Preventive Healthcare: What Messi Teaches Every Indian Family
Preventive care means seeing a doctor before a problem becomes serious. Messi’s career longevity proves its value.
Preventive healthcare includes:
Annual health check-ups
Monitoring blood pressure and sugar
Early screening tests
Vaccinations
Lifestyle counselling
Quickobook supports this approach by helping families find general physicians and specialists nearby, without long delays.
Technology in Healthcare: Changing How India Sees Doctors
Just like modern football uses data, fitness tracking, and video analysis, modern healthcare uses digital tools.
Technology in healthcare helps with:
Online appointment booking
Teleconsultation
Digital health records
Reminders for follow-ups
Better doctor-patient communication
Quickobook uses these tools to make healthcare less complicated and more human.
Mental Health: An Often Ignored Lesson from Sports
Top athletes work with psychologists to manage stress, pressure, and expectations. Messi is no exception.
In daily life, mental health is often ignored due to stigma or lack of access. Quickobook helps people find mental health professionals discreetly and easily, promoting balanced well-being.
Why Trust Matters in Both Football and Healthcare
Messi trusts his coaches, doctors, and physiotherapists. This trust allows him to focus on performance.
Similarly, patients need:
Verified doctors
Transparent information
Honest reviews
Clear communication
Quickobook builds trust by listing verified doctors and patient feedback, helping users make informed choices.
From Stadiums to Clinics: The Same Winning Formula
The same formula that builds champions also builds healthy communities:
Early action
Expert guidance
Consistency
Discipline
Right use of technology
Quickobook applies this formula to Indian healthcare, inspired by stories like Lionel Messi’s.
When to See a Doctor: Don’t Delay
You should book a doctor appointment if you have:
Persistent pain
Fever lasting more than 3 days
Sudden weight loss
Breathing difficulty
Mental stress or anxiety
Chronic lifestyle conditions
Early consultation saves money, time, and health.
Risks of Delayed Healthcare
Ignoring symptoms can lead to:
Complications
Longer treatment
Higher medical costs
Hospitalisation
Permanent damage
Messi’s early treatment prevented long-term problems. The same principle applies to everyone.
Lifestyle Lessons from Lionel Messi
Messi’s lifestyle focuses on balance:
Healthy diet
Regular exercise
Proper sleep
Stress management
Doctors available on Quickobook can help guide patients toward healthier routines suited to Indian lifestyles.
Conclusion
Lionel Messi’s life proves that talent alone is not enough. Timely medical care, discipline, and access to experts play a key role in long-term success. In the same way, Quickobook is changing how Indians approach healthcare by improving healthcare access through technology in healthcare.
Whether you are managing a condition or simply staying healthy, the right doctor at the right time can make all the difference.
Quickobook Call to Action
Book verified doctors near you
Avoid long waiting lines
Manage your health digitally
Take control of your well-being today with Quickobook
Frequently Asked Questions
Q1. Who is Lionel Messi?
A. Lionel Messi is a world-famous footballer known for skill, discipline, and consistency.
Q2. What health issue did Messi face as a child?
A. He had growth hormone deficiency, treated with early medical care.
Q3. Why is Messi’s story relevant to healthcare?
A. It shows how early access to treatment can change lives.
Q4. What is Quickobook?
A. Quickobook is a digital platform to book doctor appointments easily.
Q5. How does Quickobook improve healthcare access?
A. It connects patients with doctors quickly using technology.
Q6. Is Quickobook available in India?
A. Yes, it is designed for Indian healthcare needs.
Q7. Can I book general physicians on Quickobook?
A. Yes, you can book general and specialist doctors.
Q8. Does Quickobook reduce waiting time?
A. Yes, it helps schedule appointments in advance.
Q9. What is preventive healthcare?
A. It means seeing doctors early to avoid serious illness.
Q10. Why is preventive care important?
A. It reduces complications and healthcare costs.
Q11. How does technology help healthcare?
A. It simplifies booking, follow-ups, and communication.
Q12. Can Quickobook help with mental health?
A. Yes, mental health professionals are available.
Q13. Is Quickobook suitable for families?
A. Yes, it supports healthcare for all age groups.
Q14. Does Messi focus on mental fitness?
A. Yes, mental strength is key in professional sports.
Q15. Can regular check-ups prevent disease?
A. Yes, many conditions are manageable if detected early.
Q16. Is online doctor booking safe?
A. Yes, when using verified platforms like Quickobook.
Q17. How often should adults see a doctor?
A. At least once a year for routine check-ups.
Q18. What conditions need immediate consultation?
A. Chest pain, breathlessness, and severe fever.
Q19. Can lifestyle changes improve health?
A. Yes, diet, exercise, and sleep make a big difference.
Q20. Does Quickobook support follow-ups?
A. Yes, it helps maintain continuity of care.
Q21. Why is trust important in healthcare?
A. It improves treatment outcomes and patient comfort.
Q22. How does Quickobook verify doctors?
A. Through qualification and registration checks.
Q23. Can rural patients use Quickobook?
A. Yes, availability depends on nearby doctors.
Q24. Does Quickobook offer teleconsultation?
A. Many doctors provide online consultations.
Q25. What lesson does Messi teach about discipline?
A. Consistency leads to long-term success.
Q26. Is delayed treatment risky?
A. Yes, it can worsen health conditions.
Q27. Can Quickobook help with chronic diseases?
A. Yes, it helps manage regular doctor visits.
Q28. Why is early diagnosis important?
A. It prevents complications and improves outcomes.
Q29. Does Quickobook save time?
A. Yes, by reducing clinic waiting hours.
Q30. Is healthcare access a problem in India?
A. Yes, especially due to delays and lack of awareness.
Q31. Can technology replace doctors?
A. No, it supports doctors, not replaces them.
Q32. Does Messi follow a strict routine?
A. Yes, for fitness and injury prevention.
Q33. Can routine help non-athletes?
A. Yes, routines improve overall health.
Q34. Are regular tests necessary?
A. Yes, for early detection of health issues.
Q35. Does Quickobook list specialists?
A. Yes, across multiple medical fields.
Q36. Is Quickobook user-friendly?
A. Yes, it is designed for easy use.
Q37. Can older adults use Quickobook?
A. Yes, with simple booking options.
Q38. What role does awareness play in health?
A. It helps people seek care early.
Q39. Does Messi’s success rely only on talent?
A. No, it also relies on medical and professional support.
Q40. Can Quickobook help in emergencies?
A. It helps find doctors quickly, but emergencies need hospitals.
Q41. Is digital healthcare the future?
A. Yes, it improves efficiency and access.
Q42. Does Quickobook show doctor reviews?
A. Yes, patient feedback is available.
Q43. Can booking online reduce stress?
A. Yes, it avoids uncertainty and delays.
Q44. Are check-ups expensive?
A. Costs vary, but prevention saves money long-term.
Q45. Can lifestyle counselling help?
A. Yes, doctors can guide healthy habits.
Q46. Does Quickobook support preventive care?
A. Yes, by encouraging regular visits.
Q47. What is the biggest healthcare lesson from Messi?
A. Never delay proper medical care.
Q48. Is healthcare a team effort?
A. Yes, between patient, doctor, and system.
Q49. Can one platform improve healthcare habits?
A. Yes, by making access easy and reliable.
Q50. How can I start using Quickobook?
A. By booking your first doctor appointment online.
Read
More










 Play Store
Play Store