Introduction
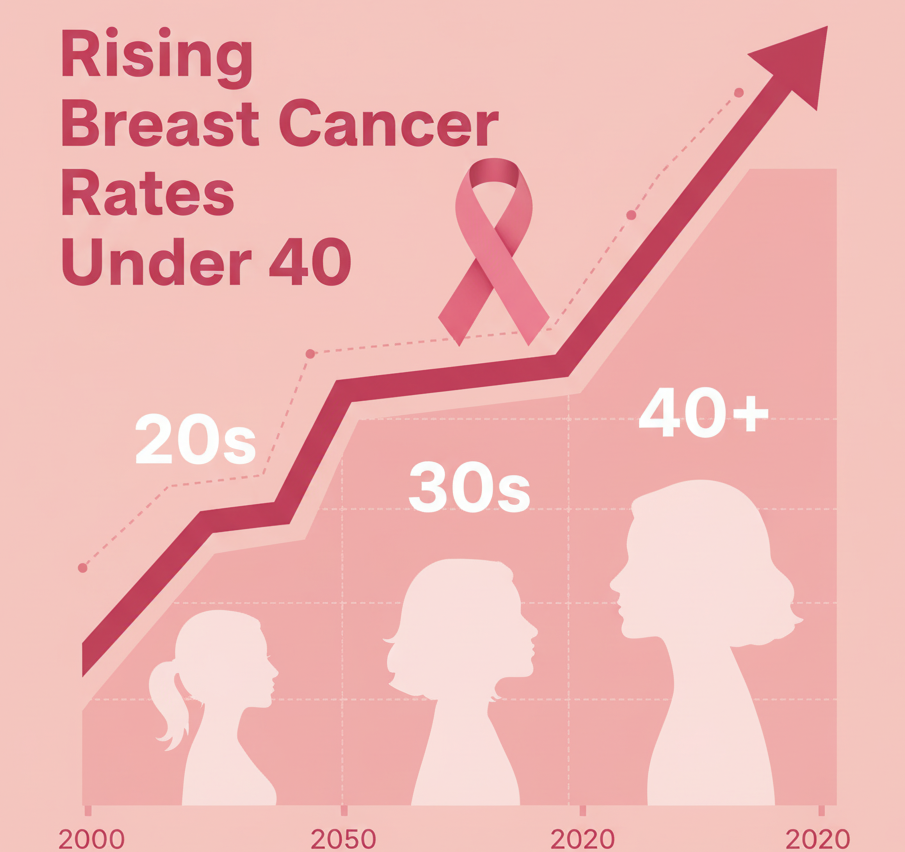
Breast cancer is no longer a disease limited to older women. In recent years, doctors across India have noticed a concerning rise in breast cancer among young women under 40. While this age group traditionally had lower risk, lifestyle changes, hormonal factors, and genetic influences have begun to shift the trend.
According to the Indian Council of Medical Research (ICMR), breast cancer has overtaken cervical cancer as the most common cancer among Indian women, accounting for over 25% of all new female cancer cases. What’s even more alarming is that nearly 20% of these cases occur in women below the age of 40.
Early detection remains the best defense — and awareness is the first step. This blog from Quickobook explains why breast cancer is affecting younger women, what early warning signs to watch for, and how you can reduce your risk through screening, lifestyle changes, and timely medical advice.

What Is Breast Cancer?
Breast cancer occurs when abnormal cells in the breast grow uncontrollably, forming a lump or mass. These cells may invade surrounding tissues or spread (metastasize) to other body parts, such as lymph nodes, lungs, or bones.
Breast tissue contains milk ducts, lobules, and fatty connective tissue. Most cancers begin in the ducts (ductal carcinoma) or lobules (lobular carcinoma). Detecting these changes early through self-examination or mammography can dramatically improve survival rates.
Why Are More Young Women Getting Breast Cancer?
Traditionally, breast cancer risk increased with age. However, multiple studies now show a sharp rise in cases under 40, especially in urban India. Experts suggest this increase is linked to a combination of lifestyle, genetic, and hormonal factors.
1. Lifestyle and Environmental Factors
- Sedentary habits and lack of exercise
- Obesity and high body fat percentage
- High intake of processed or fatty foods
- Alcohol consumption and smoking
- Late-night work shifts and poor sleep patterns
2. Hormonal and Reproductive Factors
- Early onset of menstruation or late menopause
- Delaying childbirth beyond 30
- Fewer pregnancies or no breastfeeding
- Long-term use of hormonal contraceptives or fertility treatments
3. Genetic Factors
- Mutations in BRCA1 and BRCA2 genes significantly raise risk.
- A family history of breast or ovarian cancer increases personal risk.
- Genetic counseling is recommended for women with affected relatives.
4. Stress and Urban Lifestyle
Chronic stress, exposure to pollutants, and lack of routine health checks also play subtle but significant roles.
Early Symptoms of Breast Cancer
Recognizing early warning signs can save lives. Doctors urge self-awareness and monthly breast self-examinations starting in the 20s.
Watch for these symptoms:
- A lump or thickening in the breast or underarm
- Changes in breast size, shape, or symmetry
- Dimpling or puckering of breast skin
- Nipple discharge (especially bloody)
- Nipple retraction or inversion
- Redness, swelling, or rash on the breast
- Persistent pain in one breast
Remember: not every lump is cancerous — but every new lump should be checked by a doctor.
Diagnosis and Screening
Early detection significantly improves treatment outcomes. Diagnostic steps include:
1. Clinical Breast Examination (CBE)
Your doctor checks for lumps or skin/nipple changes. This should be done yearly after age 25.
2. Mammogram
A low-dose X-ray that can detect tumors before they are felt. For high-risk women, screening may start at 30.
3. Breast Ultrasound
Helpful for women with dense breast tissue (common under 40).
4. MRI (Magnetic Resonance Imaging)
Recommended for those with strong family history or BRCA mutations.
5. Biopsy
A small tissue sample is removed and tested for cancer cells — confirming the diagnosis.
Treatment Options for Young Women
Treatment depends on the cancer’s type, stage, and hormone receptor status. Common approaches include:
- Surgery – Lumpectomy (removal of tumor) or mastectomy (removal of whole breast)
- Chemotherapy – Kills fast-growing cancer cells
- Radiation Therapy – Targets cancer cells post-surgery
- Hormone Therapy – For hormone-sensitive cancers (e.g., Tamoxifen)
- Targeted Therapy – Uses drugs that block specific cancer cell growth signals
Note: Treatment plans and drug dosages vary. Always follow your oncologist’s advice.
Lifestyle and Recovery After Treatment
Post-treatment care is vital for physical and emotional recovery.
- Eat a balanced diet rich in antioxidants and fiber
- Exercise regularly under medical guidance
- Avoid alcohol and smoking
- Practice meditation, yoga, or journaling to manage stress
- Attend regular follow-ups to monitor recurrence
- Seek counseling or join breast cancer support groups
Prevention: How Young Women Can Reduce Risk
While not all cases are preventable, you can significantly lower risk through these steps:
- Maintain a healthy weight
- Breastfeed your child (reduces lifetime risk)
- Limit alcohol intake
- Avoid long-term hormone therapy unless necessary
- Eat a plant-rich diet (green vegetables, whole grains, fruits)
- Exercise at least 30 minutes daily
- Schedule annual clinical breast exams after 25
- Perform monthly self-exams after menstruation
ALSO READ: Magnesium For Better Sleep: Benefits, Deficiency Signs, And Natural Sources
When to See a Doctor
You should consult a gynecologist or oncologist immediately if:
- You feel a lump or notice unusual breast changes
- There’s nipple discharge or persistent pain
- You have a family history of breast cancer
- You are planning pregnancy with BRCA gene risk
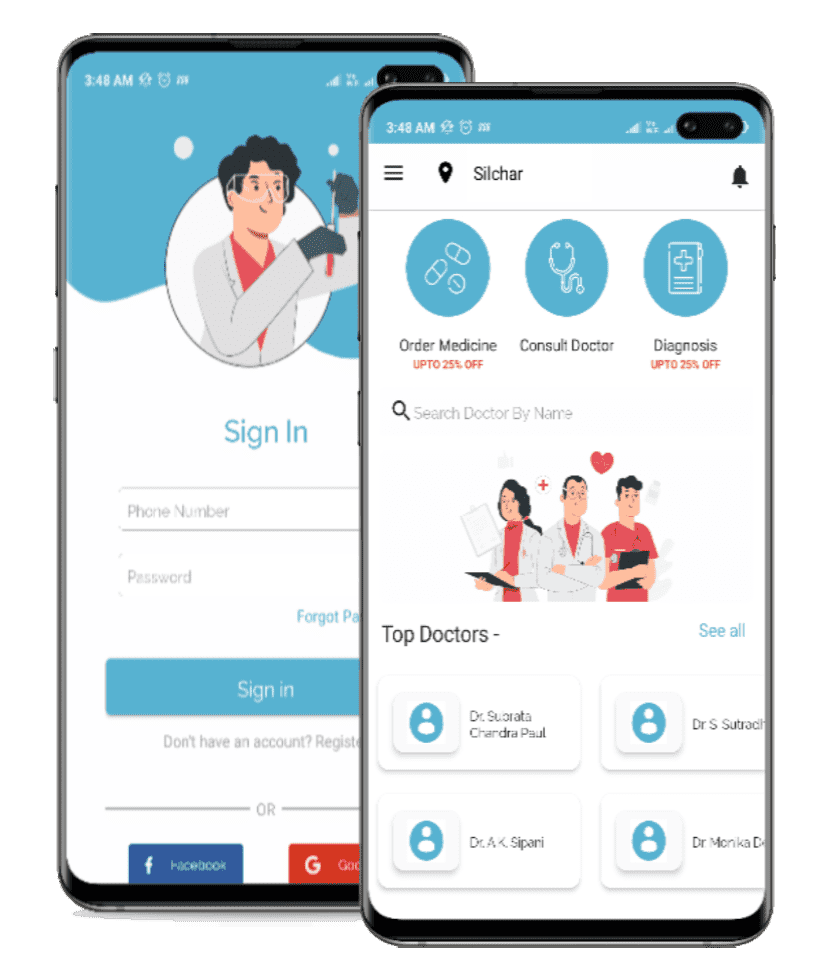
Quickobook can help you find a trusted breast specialist near you for early evaluation.
Risks and Complications
If untreated, breast cancer can:
- Spread to bones, lungs, liver, or brain
- Cause chronic pain or fatigue
- Affect fertility and hormonal balance
- Lead to depression or anxiety
However, when detected early, 5-year survival rates exceed 90% in India’s top oncology centers.
50 Expert FAQs on Breast Cancer in Young Women
Q1. What is the average age for breast cancer in India?
A: The median age is 47, but cases in women under 40 are increasing rapidly.
Q2. Can breast cancer occur at 25?
A: Yes, though rare, it’s possible—especially with genetic risk factors.
Q3. What are early warning signs?
A: Lumps, nipple discharge, or skin changes are early indicators.
Q4. Is breast pain always cancer?
A: No. Most breast pain is hormonal, but new or persistent pain needs evaluation.
Q5. How can I self-examine my breasts?
A: Use your fingertips in circular motions monthly after your period ends.
Q6. Does family history matter?
A: Yes, close relatives with breast or ovarian cancer increase your risk.
Q7. What is BRCA testing?
A: A genetic test detecting mutations that heighten cancer risk.
Q8. How often should women under 40 get checked?
A: Annual clinical exams and monthly self-checks are recommended.
Q9. Are mammograms safe for young women?
A: Yes, when done for medical reasons, radiation exposure is minimal.
Q10. Can breastfeeding prevent breast cancer?
A: Yes, it offers natural protection by regulating hormones.
Q11. Can men get breast cancer?
A: Rarely, but yes — about 1% of cases occur in men.
Q12. What foods help prevent breast cancer?
A: Leafy greens, turmeric, soy, and whole grains may help lower risk.
Q13. Is breast cancer curable?
A: Yes, if detected early and treated promptly.
Q14. Can stress cause breast cancer?
A: Stress doesn’t directly cause it but may worsen hormone imbalances.
Q15. What is triple-negative breast cancer?
A: A type that lacks three key receptors; often more aggressive.
Q16. Does obesity increase risk?
A: Yes, especially after menopause or with sedentary lifestyle.
Q17. Can young mothers get breast cancer?
A: Yes, though pregnancy slightly reduces long-term risk.
Q18. Are mammograms painful?
A: Mild discomfort may occur, but it’s brief and tolerable.
Q19. Can birth control pills cause breast cancer?
A: Long-term use may slightly increase risk; discuss alternatives with your doctor.
Q20. What is a benign lump?
A: A non-cancerous growth like a fibroadenoma; still needs monitoring.
Q21. How soon should I see a doctor after finding a lump?
A: Immediately — don’t wait for pain or changes.
Q22. Is nipple discharge always serious?
A: Not always, but bloody or one-sided discharge must be checked.
Q23. Can diet reverse breast cancer?
A: No, but a healthy diet supports recovery and immunity.
Q24. What tests confirm cancer?
A: Biopsy is the gold standard for confirmation.
Q25. What is a lumpectomy?
A: A surgery removing only the tumor and nearby tissue.
Q26. Can I work during chemotherapy?
A: Many patients do; depends on side effects and doctor’s advice.
Q27. Does hair always fall during chemo?
A: Often yes, but it grows back after treatment ends.
Q28. Is radiation therapy safe?
A: Yes, it’s precisely targeted to minimize harm to healthy tissue.
Q29. How long does treatment last?
A: Typically 6 months to 1 year, depending on stage and type.
Q30. Can yoga help recovery?
A: Yes, yoga improves flexibility, mood, and fatigue.
Q31. What is recurrence risk?
A: Some cancers can return; follow-ups detect them early.
Q32. Should I freeze my eggs before chemotherapy?
A: Yes, if you plan pregnancy later — consult a fertility specialist.
Q33. Can tattoos affect mammograms?
A: No, but always inform your technician.
Q34. Does underwire bra cause breast cancer?
A: No scientific evidence supports that myth.
Q35. Are organic foods protective?
A: They may reduce exposure to pesticides but are not a guarantee.
Q36. How does age affect survival?
A: Younger women often have more aggressive types but respond well to timely care.
Q37. Is surgery always needed?
A: Often yes, but some small tumors respond to targeted drugs.
Q38. Can I prevent it with supplements?
A: Only Vitamin D and antioxidants show mild protective benefits.
Q39. Are there warning apps or tools?
A: Yes, apps like Quickobook’s help schedule screening reminders.
Q40. What is a PET scan?
A: It shows if cancer has spread beyond the breast.
Q41. Can Ayurvedic medicine cure cancer?
A: No, but supportive herbal care may aid recovery when combined with modern treatment.
Q42. Can men carry BRCA genes?
A: Yes, and they can pass it to daughters or sons.
Q43. Can weight loss reduce recurrence?
A: Yes, maintaining healthy weight lowers relapse risk.
Q44. How can I emotionally cope?
A: Join support groups, therapy, or mindfulness programs.
Q45. What if I can’t afford treatment?
A: Government schemes and NGOs offer free or subsidized care.
Q46. How does Quickobook help patients?
A: You can find verified oncologists, compare consultation fees, and book appointments online.
Q47. Are breast cancers in India different from Western types?
A: Indian cases often present at later stages — hence early screening is vital.
Q48. Can teenagers get breast cancer?
A: Extremely rare but possible; lumps should still be checked.
Q49. How do I reduce anxiety before tests?
A: Deep breathing, talking to loved ones, and clear information help.
Q50. What is the survival rate for early breast cancer?
A: Over 90% when detected early and treated promptly.
Quickobook Call-to-Action
Don’t ignore breast changes — book an appointment with a gynecologist or oncologist near you through Quickobook.







Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment