Introduction
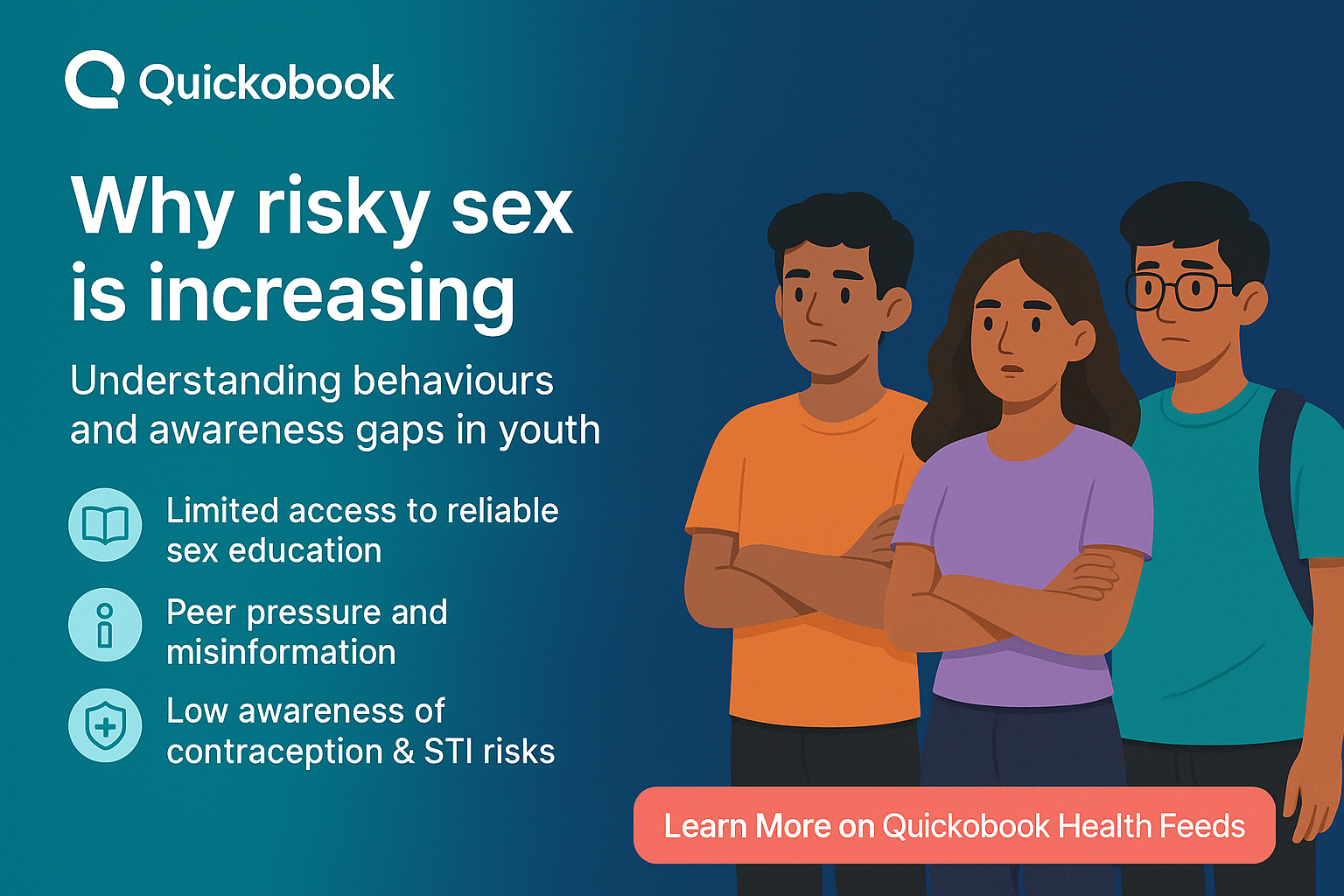
Across India, more young people are becoming sexually active than ever before. With growing exposure to social media, shifting relationships, and urban lifestyles, sexual behaviour among youth is changing rapidly. But one worrying trend stands out—unprotected sex is rising sharply among young Indians. Many engage in sexual activity without condoms or reliable contraception, often due to lack of sexual awareness, social stigma, wrong information, or impulsive decisions.
This rise is leading to serious consequences: higher rates of unintended pregnancy, sexually transmitted infections (STIs), emotional stress, anxiety, shame, and long-term reproductive health issues. While sex itself is a natural part of life, young people need correct information to stay safe, healthy, and responsible.
This detailed guide explains why unprotected sex is increasing among Indian youth, the health risks involved, myths that mislead young adults, early warning signs to watch for, ways to prevent complications, and how sexual awareness can empower young people to make safer choices.
Understanding Unprotected Sex Among Indian Youth
What unprotected sex means
Unprotected sex refers to sexual activity without using condoms, dental dams, or reliable methods of contraception. It includes vaginal, oral, or anal sex without any protective barrier. Many young people believe that “just once” is safe, but even a single unprotected encounter can cause pregnancy or transmit STIs.
Why sexual awareness matters
Most problems related to unsafe sex come from lack of knowledge. Sexual awareness means understanding how pregnancy happens, how STIs spread, what protection methods exist, and why regular check-ups matter. Without this awareness, youth make decisions that can harm their physical and emotional health.
Why Unprotected Sex Is Increasing Among Young Indians
Lack of proper sexual awareness
Many Indian schools still do not provide detailed, practical sex education. Young people either learn incomplete information from friends, social media, or pornography. This misinformation creates dangerous assumptions like:
-
“Withdrawal is safe.”
-
“You can’t get pregnant the first time.”
-
“Only people with many partners get STIs.”
-
“Oral sex is safe without condoms.”
Without basic knowledge of protection, youth take risks without understanding consequences.
Stigma and embarrassment around buying condoms
In India, many young adults feel judged when purchasing condoms. Shopkeepers may stare, ask uncomfortable questions, or show disapproval. This shame leads many to avoid using condoms altogether. Even educated youth struggle with this cultural barrier, especially in smaller towns.
Growing popularity of dating apps and casual relationships
Apps like Tinder, Bumble, and Instagram interactions make it easier for youth to form quick connections. With more casual or short-term relationships, many young Indians engage in impulsive sex. Without planned protection, these encounters often happen unprotected.
Myths and misinformation surrounding protection
Myths spread faster than facts among the youth. Common myths include:
-
“Condoms reduce pleasure, so better not use them.”
-
“It’s safe if we trust each other.”
-
“STIs are rare.”
-
“Taking a shower after sex prevents pregnancy.”
Such beliefs create a false sense of safety.
Alcohol and substance use
Parties, college events, and nightlife often involve alcohol. Under the influence, judgment drops, and decisions become impulsive. Many unprotected encounters happen because condoms were not planned or remembered.
Trust in long-term partners without testing
Couples in long-term relationships often stop using condoms after a few months, assuming they are safe. But many do not get tested before going condom-free. Without medical screening, the risk of silent infections becomes high.
ALSO READ: Early Signs Of Stis In Men And Women You Should Watch For
Limited access to contraception
Young people, especially in rural or semi-urban areas, struggle with:
-
Lack of privacy
-
Fear of judgment
-
Limited stock in nearby pharmacies
-
High cost of some contraceptives
-
No youth-friendly clinics
This lack of access increases unsafe choices.
Influence of pornography
Porn rarely shows condom use, and many youth imitate what they see. This creates unrealistic expectations and unsafe habits.
Lack of conversations at home
Parents rarely discuss sexual health due to cultural discomfort. With no one to guide them, youth rely on peers and online content, which may be inaccurate.
Health Risks of Unprotected Sex
Sexually transmitted infections (STIs)
Unprotected sex is the main cause of STIs among youth. Common infections include:
-
Chlamydia
-
Gonorrhea
-
Syphilis
-
Human Papillomavirus (HPV)
-
Genital herpes
-
Trichomoniasis
Many STIs show no early symptoms but still cause damage.
Unintended pregnancy
A single unprotected encounter can lead to pregnancy. The physical, emotional, financial, and social pressure placed on young women is often overwhelming. Many resort to unsafe abortions, especially when they fear judgment.
Emotional and mental health impact
Unprotected sex often results in:
-
Fear of pregnancy
-
Anxiety while waiting for test results
-
Guilt or shame
-
Loss of trust between partners
-
Relationship problems
-
Trauma after risky experiences
Long-term reproductive complications
Untreated STIs can lead to:
-
Infertility
-
Pelvic inflammatory disease
-
Chronic pelvic pain
-
Ectopic pregnancy
-
Complications during future pregnancies
For men, untreated infections can affect sperm count and sexual performance.
Early Warning Signs of STIs That Youth Often Ignore
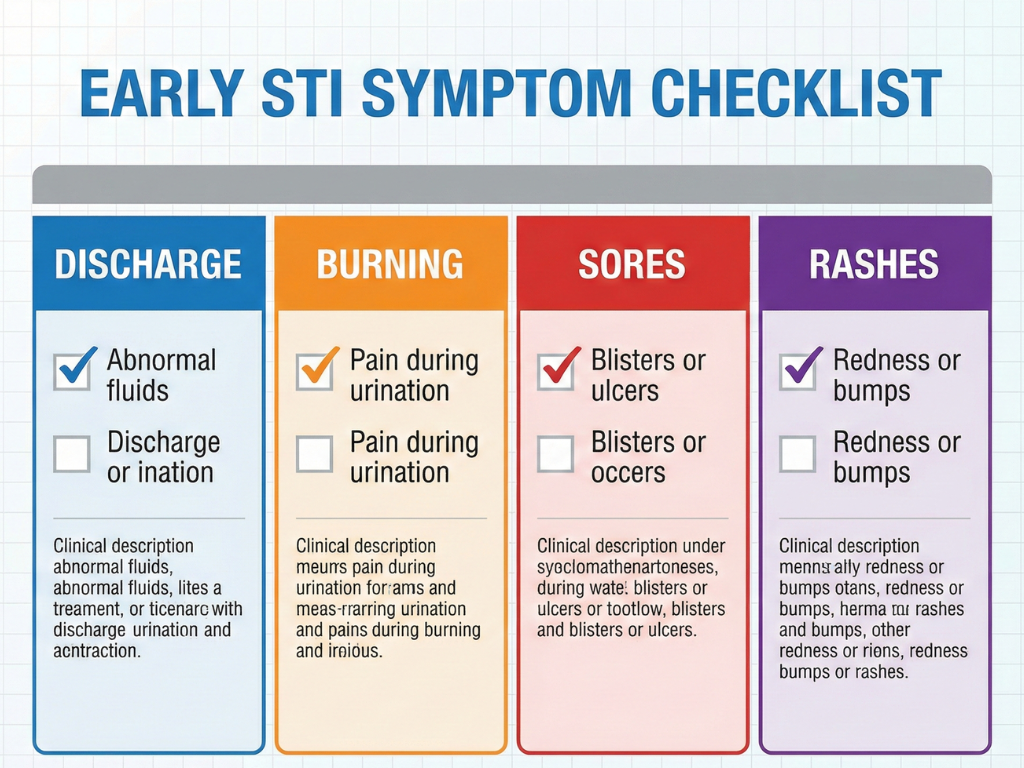
Signs in men and women
-
Burning sensation while urinating
-
Unusual discharge from penis or vagina
-
Pain during sex
-
Lower abdominal pain
-
Rashes or bumps on genitals
-
Itching around the genital area
-
Fever or body aches
-
Bleeding between periods (women)
-
Sores, ulcers, or painful blisters
Silent infections
Some infections like Chlamydia, HPV, and HIV can stay quiet for months or even years. This is why many young people unknowingly transmit infections to partners.
Why youth ignore symptoms
-
Fear of being judged
-
Assuming symptoms will go away
-
Lack of awareness
-
Embarrassment about seeing a doctor
-
Misunderstanding early signs as normal irritation
Ignoring early signs can lead to severe complications later.
Diagnosis and Testing for Young People
Common tests doctors recommend
-
Urine tests for bacterial infections
-
Blood tests for HIV, syphilis, hepatitis
-
Swab tests for vaginal or urethral infections
-
HPV screening (especially for women)
-
Rapid antigen tests for some STIs
Tests are safe, quick, private, and affordable in most cities.
Why testing matters
-
Detects silent infections
-
Prevents spreading to partners
-
Allows early treatment
-
Protects long-term reproductive health
-
Builds open communication and responsibility in relationships
Treatment Options for STIs or Complications
Medications
-
Antibiotics for bacterial STIs
-
Antiviral medicines for herpes
-
Antiretroviral therapy for HIV
-
Topical creams for mild infections
Emergency contraception
If pregnancy is a risk, emergency pills must be taken within 72–120 hours depending on the type. Only a doctor can recommend dosage.
Partner treatment
If one partner is infected, both must be treated to avoid reinfection.
Follow-up
Doctors may recommend retesting after a few weeks to ensure complete recovery.
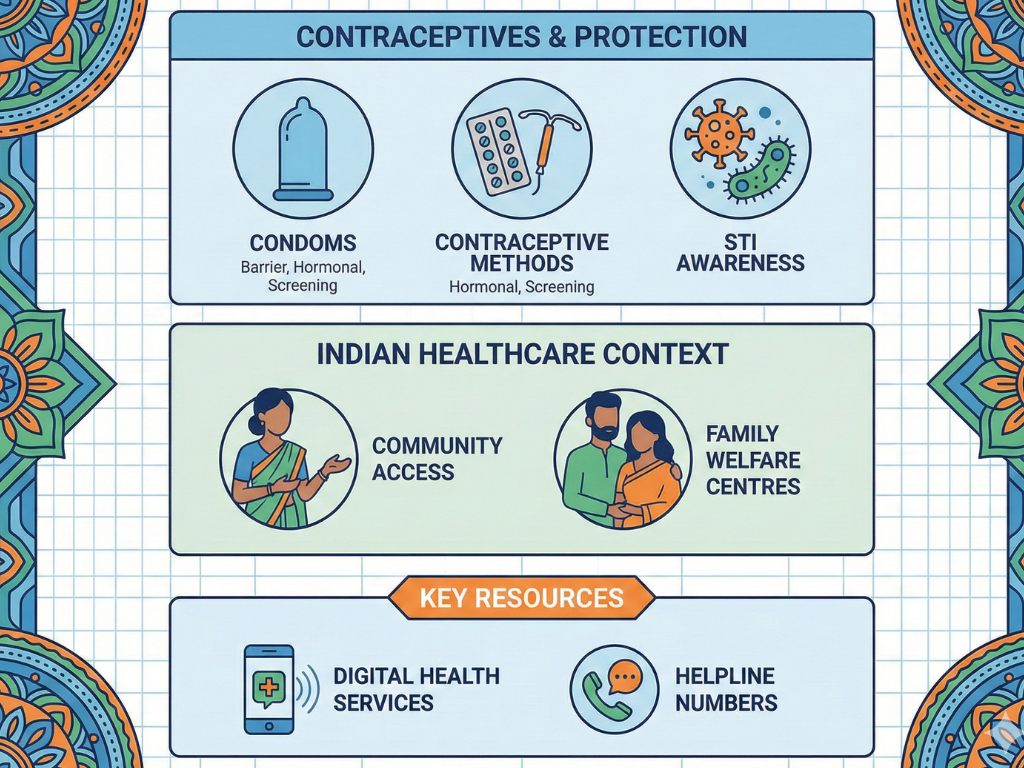
Prevention: Building Strong Sexual Awareness in Youth
Using condoms every time
Condoms protect against both pregnancy and infections. They are cheap, accessible, and highly effective when used correctly.
Regular sexual health check-ups
Youth with new or multiple partners should get tested every 3–6 months.
Open conversations with partners
Talking about protection builds trust and prevents risky decisions.
Avoiding sex under alcohol or drug influence
Clear thinking is necessary for responsible choices.
Understanding consent
Consent must be:
-
Clear
-
Free from pressure
-
Sober
-
Revocable at any time
Breaking myths with real facts
Youth must rely on verified medical sources, not social media rumours.
Vaccinations
HPV and Hepatitis B vaccines offer strong protection from long-term infections.
Youth-friendly clinics
These clinics offer privacy, correct information, and judgement-free guidance.
When to Seek Help from a Doctor

Seek medical help if you notice:
-
Painful urination
-
Abnormal discharge
-
Bleeding not linked to periods
-
Persistent itching
-
Pain during sex
-
Fever with genital symptoms
-
Sores or unusual bumps
If you had unprotected sex recently, a preventive consultation can stop problems before they start.
Major Risks and Complications If Ignored
-
Permanent infertility
-
Chronic pelvic pain
-
Spread of infections to partners
-
HIV-related complications
-
Repeated miscarriages
-
Emotional trauma
-
Long-term infections becoming harder to treat
The earlier the treatment, the better the recovery chances.
Conclusion
The rise of unprotected sex among young Indians is a complex issue shaped by social stigma, poor sexual awareness, misinformation, dating culture, lack of access to contraception, and emotional pressure. While physical intimacy is a natural part of life, safety must always come first. Youth need correct information, easy access to protection, and supportive healthcare systems to make informed choices.
By promoting sexual awareness, encouraging safe sex practices, and removing shame around discussing sexual health, we can protect the next generation from avoidable health risks and emotional distress.
Unprotected sex should never be taken lightly. Knowledge, responsibility, and open communication are the real sources of safety.
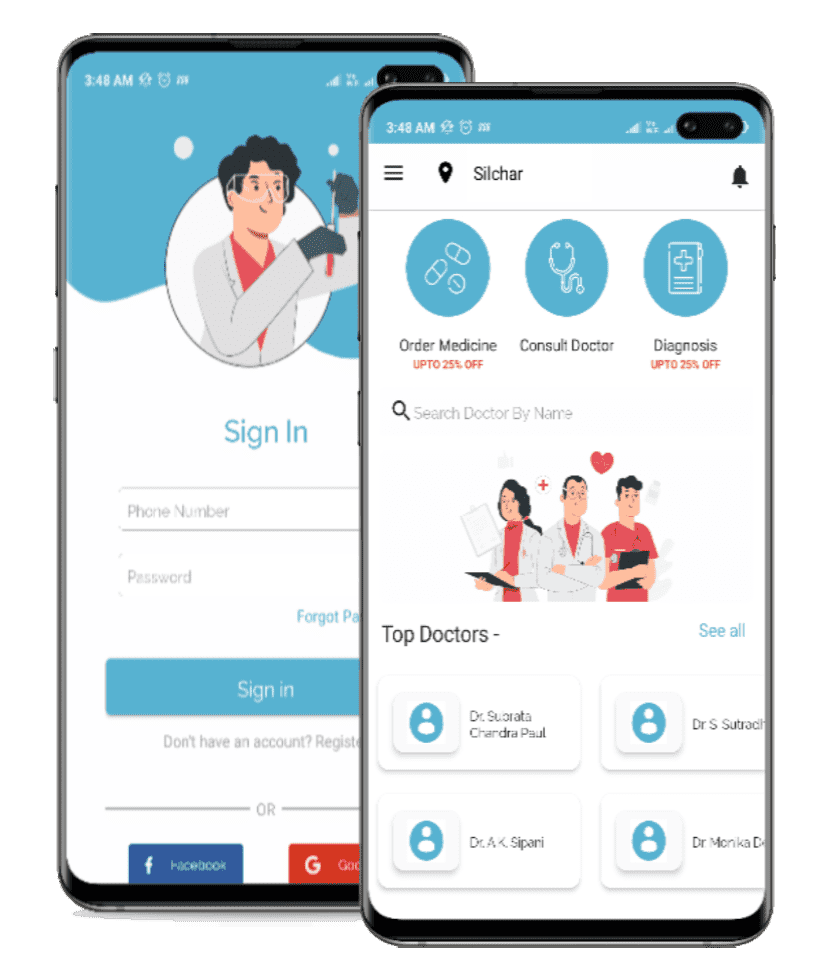
Quickobook Call-to-Action
Need private, judgment-free health advice?
Book fast and confidential appointments with expert gynecologists, urologists, and general physicians on Quickobook.
Trusted doctors. Zero embarrassment. Complete privacy.
Disclaimer
This blog is for educational purposes only and does not replace medical advice. Always consult a qualified doctor for diagnosis, treatment, or health concerns.







Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment